Cyst Aspiration
A cyst is a membranous sac or cavity of abnormal character containing fluid.
Indications for an Oral Cyst Aspiration
For a jaw bone cyst lesion or any large soft tissue oral mucogingival cyst, aspirate the cyst aspiration. To help diagnosis of erythematous, pseudomembranous candidiasis, or suspected herpetic lesions use exfoliative cytology.
Like what you’re learning? Download a brochure for our online, postgraduate Oral Pathology and Radiology certificate program.
Common Adverse Effects
Needle aspiration of fluid from a cyst rarely causes complications and generally has no contraindications assuming normal healing and clotting tendencies are present. Infection is always possible, but it is highly unlikely and can be treated with antibiotics.
There are no contraindications for exfoliative cytology, but keep in mind that it is not acceptable as a way of definitively diagnosing dysplastic and neoplastic cell changes for oral lesions.
3 Times Not to Use an Oral Cyst Aspiration
- Needle aspiration of fluid from a cyst should not be confused with fine needle aspiration cytology (FNAC) of a solid or glandular lesion. With FNAC you are attempting to withdraw cells for analysis from the mass.
- Needle aspiration of fluid is illogical when dealing with a radiopaque or solid soft tissue lesion since no fluid will be aspirated.
- You also cannot withdraw cyst lining cells with any needle aspiration method to determine the cellular basis of a cyst. For this you could use a punch biopsy to collect a portion of the cyst lining.
Step-by-Step Cyst Aspiration Procedure

Before recommending a cyst aspiration or exfoliative cytology, make sure the patient does not have a bleeding abnormality and that they have normal vital signs (e.g. pulse, blood pressure, temperature). Then, based on radiographs, select the logical entry point for the aspiration needle where the bone is thinnest.
- Select the needle (20 gauge is common) and connect it to a 10 cc syringe.
- Using a standard 27 gauge needle and local dental anesthetic, anesthetize the mucosa or gingival area where you will insert the larger aspirating needle.
- Once the entry point tissue is numb, insert the 20 gauge needle through the tissue and overlying bone into the cyst.
- Once the needle is inside the cyst, withdraw fluid and then the needle.
- Apply pressure gauze until any bleeding at the entry point stops.
Additional Considerations
Do not drive the large gauge needle in and out multiple times in sensitive anatomic areas in order to avoid damage to structures, such as the IA nerve in the mandible which could lead to post-op nerve damage.
Occasionally you will find that the bone is too dense to allow needle penetration. In these cases you must lay a flap, and using a bone drill, open a small hole through which the needle can be inserted inside the cyst. Be careful not to penetrate the cyst with the bone bur.
Differential Diagnosis of Cyst Aspiration Fluids
The primary reason for a needle aspiration of fluid is to see if the radiolucent or fluctuant soft tissue lesion contains blood or pus. When it contains blood only, the chances of the lesion being due to proliferation of vascular tissues (arteries and veins) are much higher.
More importantly, controlling the bleeding that will occur when the oral biopsy is performed is hard and potentially dangerous in the case of a hemangioma or other vascular lesion. Appropriate referral should be made.
Assuming you aspirate and withdraw non-blood based fluids, the color of the fluid may be helpful in determining the nature of the lesion. For example, extraction of a light, straw-colored fluid containing cholesterol crystals (known by their characteristic “shimmering” effect in light) is consistent with a cyst-like process.
Aspiration of a whitish to pale yellow material that appears similar to pus usually reveals an odontogenic keratocyst that contains desquamated cells and keratin.
An infected cyst that has been present for a long time contains a thicker yellow/brown material that is more difficult to aspirate.
If upon aspiration a lesion feels pneumatized, this may indicate a traumatic bone cavity as opposed to a cyst, and if aspiration yields nothing this may indicate a solid tumor-like growth.
Related Reading: The Dentist’s Guide to Oral Pathology of Vesicular Ulcerative Conditions
Don’t have time to read The Dentist’s Guide to Oral Pathology of Vesicular Ulcerative Conditions? Download the checklist!

Cytologic Smear
There are several ways to deal with a suspected fungal oral infection including agar slant culture, cytologic smear with microscopic slide examination, and biopsy of infected tissue.
The primary reason you test for fungal overgrowth is to confirm the clinical diagnosis. In most situations, the agar slant approach is adequate and you have an answer in 48 hours. In cases when you want a faster answer, the cytologic smear with microscopic examination approach is better (assuming you have the stain and the microscope in-house).
Additional Considerations
- Herpetic diagnosis requires that you can sample the transudate gathered from an intact vesicle
- While exfoliative cytology can be used to look for dysplastic and neoplastic cell changes, a biopsy is the preferred method.
Step-by-Step Cytologic Smear Procedure
- Use a sterile tongue blade to rub the buccal mucosa, and or the dorsal and ventral surfaces of the tongue, or the lesion firmly.
- Spread the collected material onto a dry microscope slide containing an opaque end.
- Immediately fix material on slide using a cytospray fixative (an alcoholic fixative spray that allows quick and precise fixation of cytological specimens).
- After spraying the slide surface, allow the alcohol to evaporate so that the remaining polyglycol film protects the specimen from damage and drying out.
- Once the material is fixed it is stained (see below) and evaluated microscopically.
Staining Methods for Candidiasis
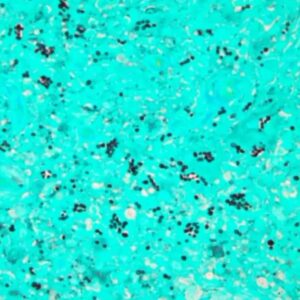
- Periodic Acid-Schiff stain (PAS).
- Papanicolaou (Pap).
- Hematoxylin and Eosin.
- Leishman methods.
The combination of the Pap-PAS staining methods is ideal for Candidiasis, while H & E staining is better for herpetic lesion diagnosis.
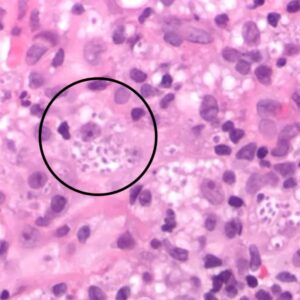
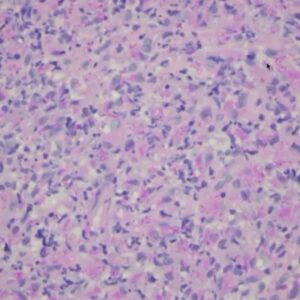
For Candidiasis, identify elongated hyphae and budding yeast or spores if present. Free-floating keratinocytes can sometimes be identified in association with candida hyphae, along with occasional inflammatory cells.
For Herpes, identify free-floating keratinocyte cells with evidence of ballooning degeneration, or viral cytopathic effect. Inflammatory cells can also be identified in some cases.
Related Reading: Oral Pathology of Secondary (Recurrent) Herpetic Eruptions
Postgraduate Oral Pathology and Radiology Certificate
Learn more about the clinical and didactic skills necessary to evaluate and manage patients with oral diseases by enrolling in Herman Ostrow School of USC’s online, competency-based certificate program in Oral Pathology and Radiology.

