OPSCC in HPV Positive vs. HPV Negative Patients
You have oral cavity squamous cell carcinoma that is still related to smoking and drinking. Because there is less male smoking and more female smoking it is evening out the incidence of squamous cell carcinoma in the oral cavity and remaining stable over time.
However, for oropharyngeal squamous cell carcinoma which is HPV related, we’re seeing an increase in males. It is usually younger than 40 years and most often associated with the high risk HPV type 16 and 18.
Don’t have time to read this article? We get it. Download the Diagnosing Vesicular Ulcerative Conditions checklist to get the key information and images from this article plus all the other conditions we cover in the Dentist’s Guide to Oral Pathology.



The first picture is a good example of an ulceration of oral cavity that was a squamous cell carcinoma. The second image is a less obvious ulceration more like a granular erythroplakia of the tonsillar pillars, soft palate area. This is a typical HPV type oropharyngeal squamous cell carcinoma.

You can think of the at-risk patient now being two populations.
First is the HPV negative patient which is your classic smoke or drink, older male with the classic high-risk sites. Second, is the population of HPV positive, younger males between 20 and 40, non-smokers non-drinkers, and usually affected at the oropharynx.
Here is a picture of squamous cell carcinoma related to HPV of the oropharynx which looks granular in appearance.
HPV Integration
HPV, like herpes, is ubiquitous. It’s all over the place. 90% of us have it. Luckily, most of us clear the infection, but there are a subset of patients that will not clear the infection.
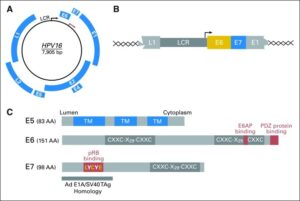
What happens is you have your HPV 16 which is one of the high-risk subtypes and they’ve got these viral oncoproteins E6 and E7 that transform epithelial cells. A portion of this virus actually gets integrated from the L1 to the E1 into our DNA. If this V represents our DNA, the virus inserts itself into our DNA. It has its own promoter so it can transcribe E6 and E7 proteins whenever it wants.
If we go down here we see the E6 and E7 proteins function in proliferation. E6 functions to halt apoptosis, which is really important for our body to naturally kill abnormal cells, but this E6 protein will stop that from happening. So proliferation and halting apoptosis causes cell immortalization and genomic instability. That’s how transformation and ultimately squamous cell carcinoma of the oral cavity related to HPV occur.
Biologic Profile of HPV-positive Tumors
It is interesting that HPV-positive tumors’ biologic profile is very different from HPV-negative. They have unique molecular profiles, related to viral oncoproteins E6 and E7 that transform epithelial cells, and they significantly overlap with HPV positive cervical carcinomas. It’s a very uniform way of cancer to develop.
Contrast that with HPV negative squamous cell carcinoma which is kind of random and related to carcinogens. In these cases, you see whole chromosome arms being deleted. It’s not nice and organized like the HPV-positive squamous cell carcinomas.
HPV Squamous Cell Carcinoma
There’s been quite a few studies that show that HPV positive oropharyngeal squamous cell carcinoma have a better survival rate than their HPV negative counterparts. For example 62% survival versus 47% within the negative tumors. In this example 2-5 years will be 91% if it’s HPV positive versus 74% if it’s HPV negative with the follow-up being five years.
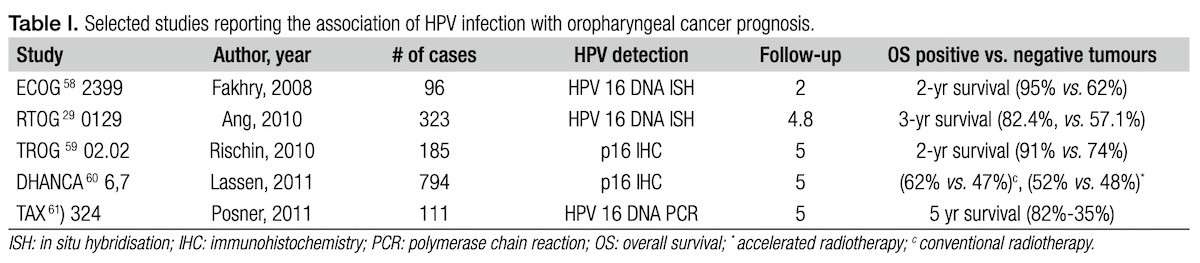
This is interesting because this leads us to think that we can treat these patients a little less aggressively. This holds true when you stratify the fact that young patients are more frequently affected by HPV positive oropharyngeal squamous cell carcinoma. If you take away all the outside factors it still holds true that there’s a better prognosis. The prognosis speaks to the fact that OPSCC develops in a more organized manner.
Also it is important to know that if younger patients that have HPV positive squamous cell carcinomas smoke or drink the better survival is negated. They will have a survival rate that more closely follows the HPV negative squamous cell carcinoma.
5-Year Survival Rates
This table provides oral cavity and oropharyngeal squamous cell carcinoma five-year survival rates compared with breast, colorectal, and melanoma. When you take into account all stages compared with melanoma, breast cancer, and colorectal carcinoma we have a worst overall 5-year survival rate. That’s not good.
When you look at melanoma for example you see that it’s overall 5-year survival rate, over all stages, reflect the local stages. What does that tell us? That tells us that people go see the dermatologist, dermatologists are aware, and they screen their patients well. That does not hold true for the oral cavity and the oropharynx.
We need to do our jobs a better. We need to perform head and neck cancer screening, examine every patient, every time, look for suspicious lesions, and biopsy suspicious lesions so we can bring our overall 5-year survival rate up to something more acceptable.
Vesicular Ulcerative Conditions
Download the Diagnosing Vesicular Ulcerative Conditions checklist to get all the key information and images from this article.

Postgraduate Oral Pathology and Radiology Certificate
Learn more about the clinical and didactic skills necessary to evaluate and manage patients with oral diseases by enrolling in Herman Ostrow School of USC’s online, competency-based certificate program in Oral Pathology and Radiology.

