As people age, their oral health becomes more complex, and one critical area of concern is the risk of oral cancer. A key part of this risk involves oral potentially malignant disorders (OPMDs)—lesions that aren’t cancerous yet but have the potential to become cancer. Another major contributor? Alcohol consumption is a well-established risk factor for several types of cancer—including those affecting the oral cavity. Even moderate drinking can significantly increase the likelihood of oral and oropharyngeal cancers, especially in older adults.
For dental professionals, especially those caring for aging patients, understanding these risks is essential for prevention, screening, and early intervention.
What Are Oral Potentially Malignant Disorders (OPMDs)?
OPMDs are abnormal patches or lesions in the mouth with a higher-than-average risk of becoming cancerous. They are often painless and may go unnoticed without a professional exam.
Common types include:
• Leukoplakia: White patches in the mouth
• Erythroplakia: Red, easily bleeding lesions
• Oral lichen planus: A chronic inflammatory condition
• Oral submucous fibrosis: Mouth stiffness, often linked to betel nut use
• Actinic cheilitis: Sun damage to the lips
• Lesions from systemic conditions: Such as lupus or graft-versus-host disease

Actinic cheilitis image (image reprinted from “Br J Oral Maxillofac Surg vol. 56, Revisiting lip shave: a solution for disorders of the vermilion border. Pages 60–63, Copyright 2019 [107] with permission from Elsevier”).
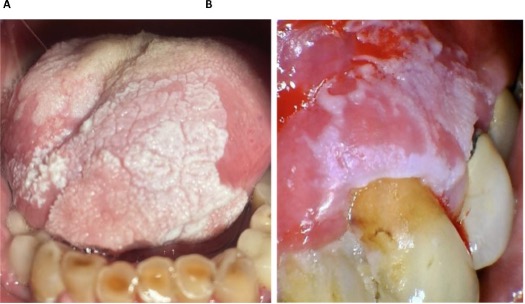
Proliferative verrucous leukoplakia. (A) 81-year-old male with a history of PVL and biopsy proven dysplasia of the tongue. (B) 69-year-old female with PVL of the left maxillary gingiva and biopsy proven dysplasia with SCC transformation (Images provided courtesy of Dr. Sedghizadeh, Ostrow School of Dentistry of University of Southern California).
Like what you’re learning? Download a brochure for our Geriatric Dentistry Master Program certificate or master’s degree program.
Alcohol: A Major, Often Overlooked Risk Factor
Established Carcinogen:
Alcohol is classified by the International Agency for Research on Cancer (IARC) as a Group 1 carcinogen, placing it in the same category as tobacco and asbestos. Its link to oral cancer is supported by decades of research. Even light drinking poses risk:
• One drink per day over five years increases the relative risk of mouth cancer by about 40%.
• Two drinks daily nearly double the risk.
• Alcohol’s metabolite, acetaldehyde, damages DNA and promotes cancer development—particularly in the oral cavity, pharynx, and larynx.
Why Older Adults Are Especially Vulnerable
Older adults often face:
• Long-term alcohol or tobacco use
• Decreased ability to repair cellular damage
• Chronic health conditions and immune changes
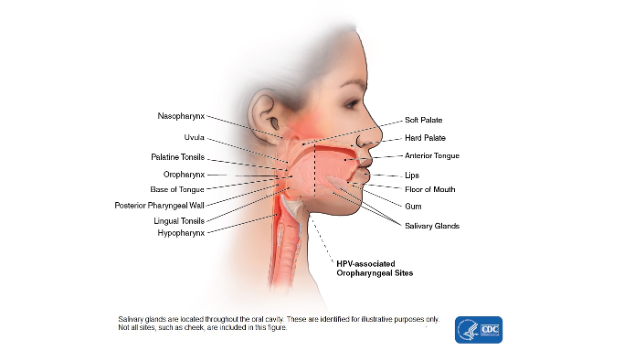
• Infection with the sexually transmitted HPV16 virus has been linked to oral cancers.
• Epstein- Barr virus can raise the risk of cancers in the nose, behind the nose, and cancers of the salivary glands.
• Genetic factors (e.g., impaired alcohol metabolism in some populations)
These cumulative factors elevate cancer risk and highlight the importance of vigilant dental care.
What Dental Professionals Can Do
1. Encourage your patients to Perform a Self-Exam Monthly
Using a bright light and a mirror:
• Any dentures should be removed.
• The individual should look and feel inside the lips and the front portion of the gums.
• They should tilt their head back to inspect and feel the roof of the mouth.
• The cheek should be pulled outward to examine its inner surface as well as the back of the gums.
• The tongue should be extended fully, allowing all its surfaces to be inspected.
• Both sides of the neck, including under the lower jaw, should be gently felt to check for any lumps or enlarged lymph nodes (glands).
2. Screen Consistently:
Many OPMDs and early-stage oral cancers are asymptomatic. Regular, thorough oral exams are critical for early detection. Watch for these signs:
• White, red, or mixed-color patches
• Persistent sores that don’t heal
• Thickened or rough areas inside the cheeks
• Difficulty opening the mouth
• Infection with the sexually transmitted HPV16
• Change in voice
3. Take Detailed Histories
Always ask about alcohol and tobacco use. Consider cultural and genetic backgrounds that might increase risk (e.g., East Asian descent with alcohol flushing response).
4. Educate Patients
Use your role as a trusted provider to counsel older patients on the risks of alcohol. Even brief interventions can influence behavior—especially when framed around cancer prevention.
5. Coordinate Care
Work with primary care physicians or specialists to create comprehensive risk-reduction plans. Reducing alcohol intake can also lower the risk for cancers of the esophagus, liver, and colon.
6. Manage and Treat Early
For patients with OPMDs, treatment may include:
• Surgical excision or laser therapy
• Photodynamic therapy
• Medications for immune-related lesions
• Lifestyle counseling to stop tobacco and alcohol use
Final Thoughts
Oral cancer prevention in older adults starts with awareness—of OPMDs, alcohol-related risks, and the power of early detection. As a dental professional, you’re in a unique position to identify warning signs, educate your patients, and collaborate with the broader healthcare team to reduce cancer risk.
Let your routine check-ups be more than cleanings—make them lifesaving.
Postgraduate Geriatric Dentistry
Are you looking for improved ways to diagnose, treat, and manage the oral healthcare of older patients? Explore our online master’s and certificate program in Geriatric Dentistry.
References
CDC Head and Neck Cancer Basics https://www.cdc.gov/head-neck-cancer/about/index.html accessed May 4, 2025
American Association of Oral and Maxillofacial Surgeons Oral Cancer https://aaoms.org/wp-content/uploads/2022/06/2017_oral_cancer_fact_sheet.pdf accessed May 4, 2025
U.S. Surgeon General. (2025) Alcohol and cancer risk. The U.S. Surgeon General’s Advisory. US: Office of the Surgeon General. https://www.hhs.gov/sites/default/files/oash-alcohol-cancer-risk.pdf
Ana Contreras, Mohsin Mahmood, Hansel Montilla, Reyes Enciso, Phuu P. Han, Piedad Suarez-Durall, Oral potentially malignant disorders in older adults: A review, Dentistry Review, Volume 3, Issue 3, 2023, 100071, ISSN 2772-5596,



