
Human Papillomavirus (HPV) is an infectious disease that can cause lesions in the genital and oropharyngeal areas. It is considered the most common sexually transmitted infection (STI) in the United States. Besides being spread horizontally between individuals, sexually or non-sexually, through skin-to-skin, skin-to-mucosa, or mucosa-to-mucosa, the virus may also be transmitted vertically from mother to child during birth or breastfeeding (Betz, 2018).
According to the Centers for Disease Control and Prevention (CDC), about 70% of oropharyngeal cancers are connected to HPV. Dentists play an important role in diminishing this number through prevention by educating patients, recommending the HPV vaccination, and doing a comprehensive intraoral and extraoral examination to recognize or suspect possible benign oral HPV lesions, especially the ones with the potential for malignant transformation.
Like what you’re learning? Download a brochure for our online, postgraduate Oral Pathology and Radiology degree program.
The HPV vaccine: a safe and efficacy way to prevent cancer
The FDA approved the 9-valent HPV vaccine (Gardasil® 9), the quadrivalent HPV vaccine (Gardasil®), and the bivalent HPV vaccine (Cervarix®) after passing through strict safety testing. In addition, clinical trials over 15 years show that the HPV vaccines are considered safe and effective (CDC, 2021).
To prevent children from having HPV-related cancers, the CDC recommends that individuals at ages 11-12 years receive two doses of the HPV vaccine, given 6 to 12 months apart. The vaccine shows more efficacy when done before the person is exposed to the virus, and it can be given starting at the age of 9 years (CDC, 2023).
Teenagers after the age of 15 years and young adults until the age of 26 years are also recommended, and they may receive three doses of the vaccine over six months (CDC, 2023).
The CDC states that the HPV vaccination is not recommended for everyone older than 26 years. However, some adults aged 27 to 45 or sometimes older may have some benefits and might choose to take the vaccine after talking to their healthcare providers and explaining their risk of acquiring new HPV infections. Due to more people over the age of 26 years possibly being already exposed to HPV, this group of individuals may have fewer benefits in receiving the HPV vaccine (CDC, 2023). The CDC does not recommend the HPV vaccination for pregnant women.
Benign HPV Oral Lesions
The common benign HPV-related lesions in the oral mucosa include squamous papilloma, condyloma acuminatum, verruca vulgaris, and multifocal epithelial hyperplasia. They appear as bumps or warts in the oral cavity and oropharynx, and they are not cancerous and most are not premalignant either (Betz, 2018).
While 70% of squamous cell carcinomas in the oropharynx are related to high risk HPV subtypes, in the oral cavity, less than 6% are HPV related. Most HPV lesions are subclinical and cleared within 1 to 2 years. However, about 0-23.1% of individuals may experience persistent infections. The incidence of HPV lesions in the oral cavity is about 3% (Betz, 2018).
Squamous papilloma (SP) is a common and the most frequent benign epithelial lesion usually associated with low-risk HPV types 6 and 11 (50%); it usually appears as a solitary, painless, soft, and pedunculated nodule with “finger-like” projections or may have a “cauliflower” or “warty” appearance (Figure 1).
- Demographics: children and adults (3rd to 7th decade)
- Color: ranges from whitish to pinkish and reddish
- Size: usually between five millimeters to one centimeter
- Location: commonly involves the soft palate/uvula, tongue, lips, gingivae, and tonsils.
- Diagnosis: Clinical diagnosis is suspected by the often papillary appearance, but flat variants exist, and an excisional biopsy is necessary for the final diagnosis
- Recurrence: is rare
- Malignant transformation: dysplasia is not common, and association with oral or oropharyngeal cancers is not known (Stojanov, 2020).

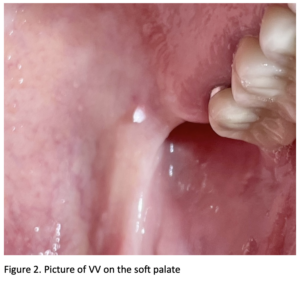
Verruca Vulgaris (VV), also known as a Common Wart, is very common on the skin, especially in the hands, and accounts for 70% of warts. Relatively uncommon in the oral cavity, the mucosal lesions resemble their cutaneous counterparts clinically. Autoinoculation is the main transmission mode (Betz, 2018).
Clinically, this exophytic lesion may present a verrucous surface, and even though it may appear in clusters, it is more often solitary (Figure 2). VV is well-defined, sessile, and asymptomatic (Betz, 2018).
Verruca Vulgaris is commonly associated with HPV types 2 and 4, and histopathological examination makes a diagnosis. Treatment of oral lesions is surgical excision, cryosurgery, or electrosurgery. However, some cases show spontaneous regression of verruca vulgaris (Neville, 2016).
- Demographics: higher incidence occurs in teenagers aged 12-16, with about 10% of children and young adults affected (Betz, 2018).
- Color: pinkish to whitish
- Size: usually less than one centimeter
- Location: the most common intraoral locations are the labial mucosa, palate, and anterior tongue
- Diagnosis: clinical diagnosis and an excisional biopsy is necessary for the final diagnosis.
- Recurrence: very low
- Malignant transformation: not seen in this type of lesion
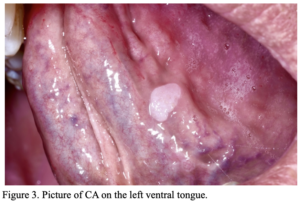
Condyloma Acuminatum (CA) is the most reported sexually transmitted infection in the United States and the United Kingdom and is normally found in the genital area. Sexual transmission may be suggested by simultaneous lesions in the genitalia and the oral cavity (Betz, 2018).
CA may be pedunculated clinically (Figure 3), but sessile lesions are more frequent and may be solitary or multiple, which may become together and form one large mass. These lesions have a “cauliflower” or mulberry surface texture (Betz, 2018).
The commonly associated HPV types for CA are the low-risk 6 and 11 and the high-risk 16 and 18, responsible for most HPV-caused cancers. Surgical excisional biopsy of this benign lesion is curative, with low recurrence (Betz, 2018).
In the case of multiple CA lesions, which are usually more common than solitary ones, multiple epithelial hyperplasia should be considered in the differential diagnosis. However, MEH is found more frequently in children and affects wider areas, while CA occurs more in adults (Betz, 2018).
- Demographics: adults are more commonly affected (3rd to 4th decades)
- Color: pinkish to whitish
- Size: usually ranges from one centimeter to one centimeter and a half, but lesions of three centimeters have been reported
- Location: the most common location in the oral cavity is the tongue and upper lips
- Diagnosis: clinical correlation and histopathological examination
- Recurrence: low recurrence
- Malignant transformation: may occur, especially if related to high-risk HPV types 16 and 18
Focal or Multifocal Epithelial Hyperplasia, also known as Heck’s Disease, is a benign condition first discovered in Native Americans and remains common in Indigenous children. In addition, genetic susceptibility may be a factor for a higher incidence in endemic areas or affecting various family members (Betz, 2018). Lower socioeconomic and overcrowded living conditions, poor hygiene, malnutrition, and HIV-positive individuals are additional factors for MEH infection (Neville, 2016).
Heck’s Disease is strongly associated with HPV types 13 and 32 and is typically characterized by multiple lesions, varying in size, and affecting different areas. These sessile lesions may have clinical presentation as papulonodular, which are flat and mucosa-like color lesions, or papillomatous, with a white and pebbly surface (Betz, 2018).
- Demographics: predominantly occurs in children and teenagers
- Color: whitish to pinkish lesions
- Size: vary from one millimeter to one centimeter
- Location: papulonodular usually occurs on the buccal and labial mucosa, whereas the papillomatous presentation is found more often on the tongue and attached gingiva
- Diagnosis: often suggested by clinical findings and demographics correlation, histopathological examination gives the final diagnosis
- Recurrence: is possible after either treatment or spontaneous regression.
- Malignant transformation: does not occur with this lesion

Conclusion
Oropharyngeal cancers related to HPV increased from 20% to 70% within the past 20 years. As healthcare providers and dentists, we should be more proactive in diminishing this number by educating our patients and recommending the HPV vaccination, as well as recognizing the possible benign HPV lesions we may encounter in the oral cavity and, especially, in the oropharynx.
Although HPV may be sexually transmitted, other ways of transmission are also possible. A safe and effective way to prevent HPV infection and the cancers that it can cause is the HPV vaccine, which is recommended for everyone from age 11-12 through the age of 26 years if not fully vaccinated already. Children of 9 years can also receive the vaccine; some adults from 26-45 may benefit from HPV immunization.
In case of prevention failure, recognizing and managing the HPV lesion is a way to control the disease. Clinical presentation and demographics suggest oral HPV lesions and histopathological examination with clinical correlation is often necessary for final diagnosis.
Postgraduate Oral Pathology and Radiology Degree
Learn more about the clinical and didactic skills necessary to evaluate and manage patients with oral diseases by enrolling in Herman Ostrow School of USC’s online, competency-based certificate or master’s program in Oral Pathology and Radiology.
References
- Betz, S. J. (2019) HPV-Related Papillary Lesions of the Oral Mucosa: A Review. Head & neck pathology (Totowa, N.J.). [Online] 13 (1), 80–90.
- CDC, HPV Vaccine Safety (2021)
- CDC, HPV Vaccine (2023)
- Stojanov, I. J. (2020) Oral Cavity & Oropharynx Benign Epithelial Tumors & Processes – Squamous papilloma (PathologyOutlines.com, Inc.)
- Neville, B. W. et al. (2016) Oral and maxillofacial pathology. 4th ed. St. Louis, Missouri: Elsevier.
