White lesions, also known as “white patches,” in the oral cavity refer to abnormal areas of the oral mucosa that have a white or whitish appearance. They may present as patches or plaques on the soft tissues inside the mouth. White lesions can arise from various causes, including chronic irritation, infection, inflammation, or potentially malignant conditions [1, 2].
These lesions can develop from benign to more serious dysplastic and cancerous lesions, making the white lesions diverse. While certain characteristic features can help differentiate these lesions, the presence of similar features can sometimes complicate the diagnosis. White lesions constitute only 5% of oral pathoses. Some white lesions like keratosis are benign or reactive, while some specific types have the potential for malignant transformation, such as Proliferative Verrucous Leukoplakia (PVL) and Oral Lichen Planus (OLP) [3].
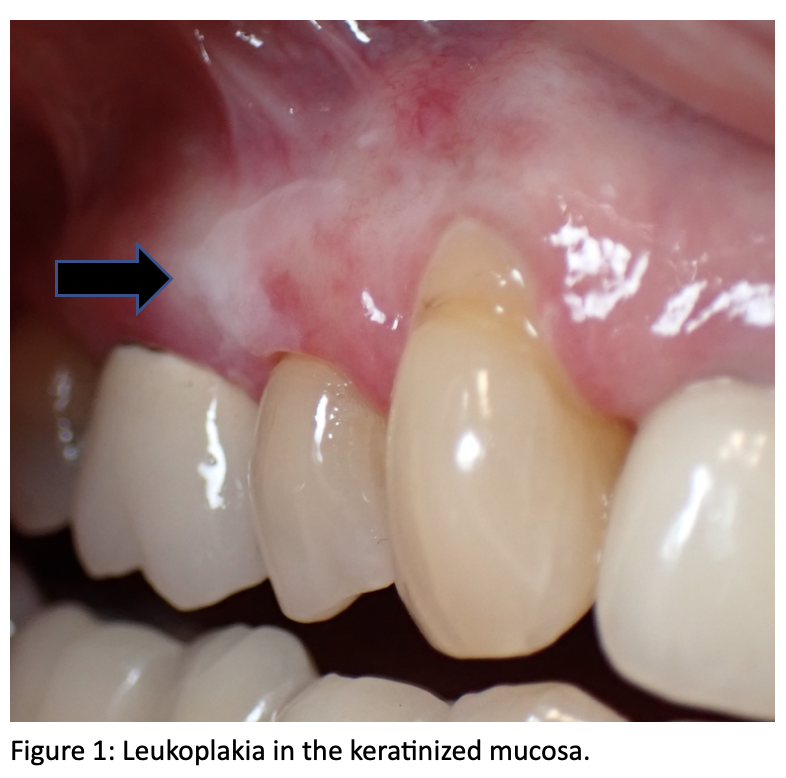
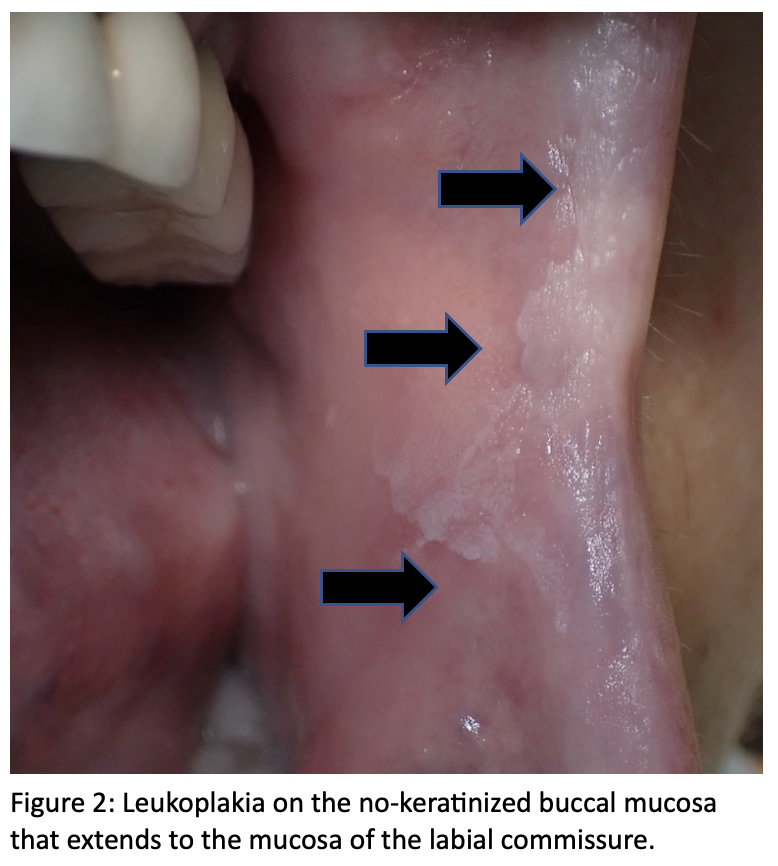
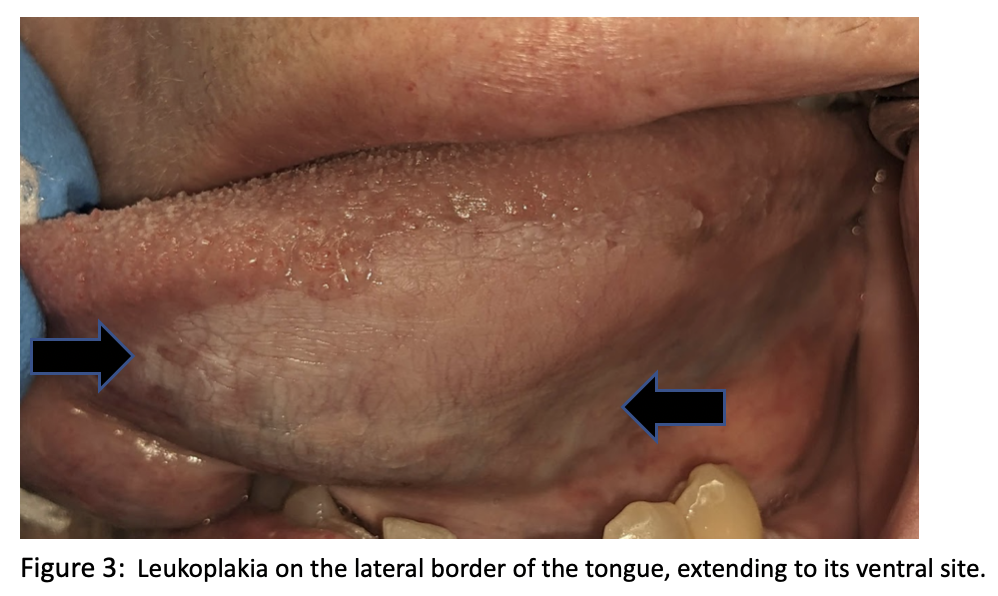
Oral leukoplakia is a term used to describe a white patch or plaque in the oral cavity that cannot be clinically or pathologically categorized as any other specific disease. Studies have shown that leukoplakia can progress into a malignant disorder in the oral cavity. Plaques, erosive and ulcerative sites, especially on the soft palate, lateral, and ventral surface of the tongue or floor of the mouth, show more tendency for harboring dysplasia or carcinoma [1,3,4].
Like what you’re learning? Download a brochure for our online, postgraduate Oral Pathology and Radiology certificate program.
Clinical features: clinically, the lesion is not wipeable; it may appear as a thin, flat to slightly elevated, white to gray plaque with a translucent, fissured, or wrinkled surface. Subsequently, the lesion may become a thick (or homogeneous) leukoplakia, appearing as a leathery, opaque, white plaque with deepened fissures.
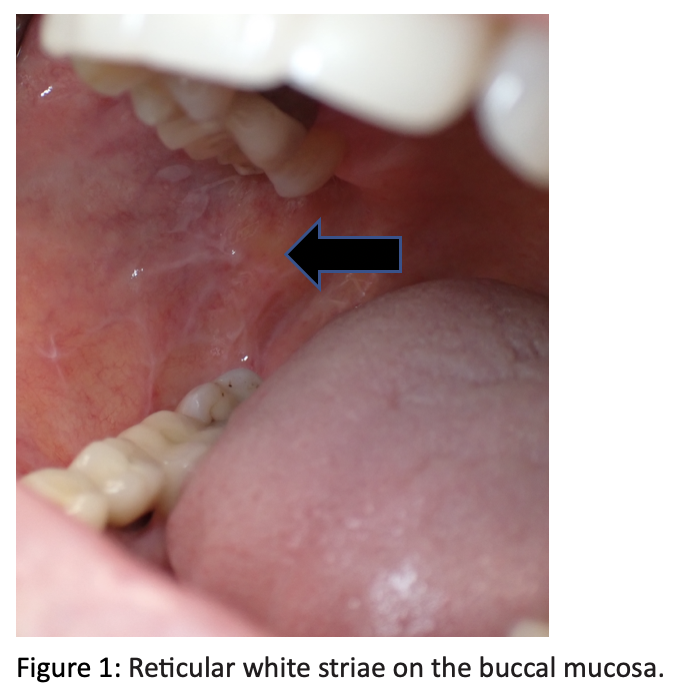
Locations: It can be found in the keratinized (Figure 1) and nonkeratinized oral mucosa (Figures 2 & 3); most patients are asymptomatic.
Risk Factors: Some authors mentioned the relationship between leukoplakia and tobacco, alcohol, sanguinaria, ultraviolet radiation, trauma, betel quid chewing, genetic factors, mate tea, and microorganisms. Around 16% to 62% of oral squamous carcinoma is related to a pre-existing leukoplakia [4,5)].
Common Differential Diagnoses
- Leukoedema
- Lichen planus
- Epithelial dysplasia
- Chemical burn
- Keratosis
Considerations: It is important to note that long-term follow-ups (for life) and biopsies should be performed to enable early diagnosis of potential malignant transformations and improve patient outcomes.
Proliferative Verrucous Leukoplakia
Proliferative verrucous leukoplakia (PVL) is a rare form characterized by progressive and multifocal “white patches” with a high rate of malignant transformation to either squamous cell cancer or verrucous carcinoma. It exhibits a predilection for women (female-to-male ratio, 2.7: 1 to 4: 1), with a mean age at diagnosis of 67 years. Even with treatment, recurrence rates range from 87% to 100%, and malignant transformation rates are >70% [1,2].
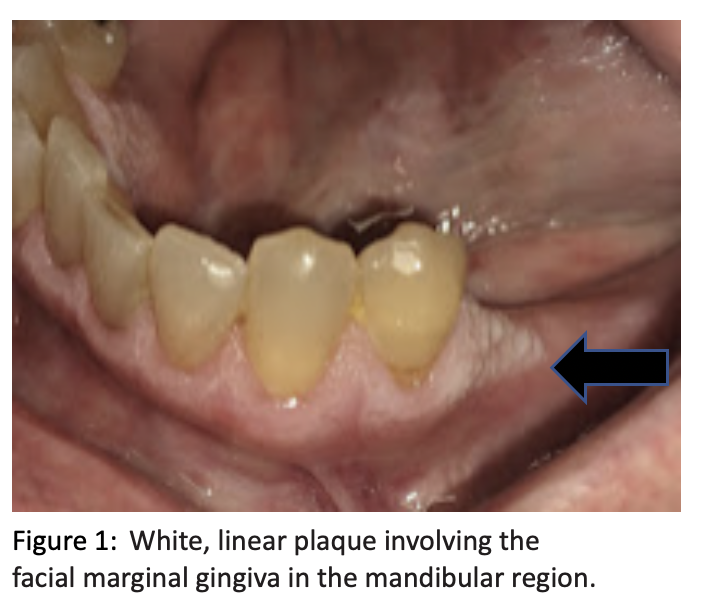
Clinical features: Initially, the patient may exhibit a solitary, homogenous white lesion that mimics conventional oral leukoplakia. Occasionally, an erythematous component also may be evident. However, the patient develops additional and/or more extensive lesions over time, often with bilateral involvement. Early lesions tend to be relatively flat, whereas older ones exhibit rough, granular, or warty surfaces.
Frequently involved sites: Frequently involved sites include the gingivae, alveolar mucosa, buccal mucosa, and tongue.
Risk Factors: Proliferative verrucous leukoplakia (PVL) is known for its progressive nature and the potential to develop into verrucous or conventional squamous cell carcinoma over time. Certain clinical signs can raise concerns about malignancy, such as erythema (redness), a warty or papillary surface, ulceration, pain, and paresthesia.
Common Differential Diagnoses:
- Epithelial Dysplasia
- Verrucous Carcinoma
- Squamous Papilloma
- Verrucous Hyperplasia
- Nodular Leukoplakia
Considerations: Proliferative verrucous leukoplakia-associated cancer mortality rates reportedly are 39-43%. It is important to closely monitor such cases, as early detection and intervention can significantly impact the prognosis. Long-term follow-ups, biopsy, and vigilant observation of lesion progression and recurrence are crucial in managing PVL and identifying potential malignant transformation.
Oral Lichen Planus
Lichen planus (LP) is defined as a common chronic mucocutaneous disease, the exact cause of oral lichen planus is unknown, but it is believed to be an immune-mediated disorder. Etiology studies (OLP) involve 0.1–2.2% of the general population and mostly arise after middle age, with a mean age of 55. Women are affected more frequently than men, with a female-to-male ratio 3:2 [3,4].
Clinical features: OLP can be present in Reticular form: characterized by the painless, symmetric distribution of interlacing white lines (Wickham’s striae), sometimes with small white papules or plaques, on the posterior buccal mucosa. Erosive form: painful, shallow ulcers that can vary in size, surrounded by a zone of erythema with fine radiating white striae at the periphery, and in severe cases, the condition may wax and wane and be presented as a lichenoid reaction.
Frequently involved sites: OLP occurs most frequently on the buccal mucosa, gingivae, tongue, and skin; nails and the GU tissues may or may not be involved.
Risk Factors: Autoimmune disorders, allergic reactions, genetic predispositions, certain medications, and stress can contribute to flare-ups or exacerbations of oral lichen planus (OLP).
Differential Diagnosis Considerations:
- Lichenoid drug reaction
- Mucous Membrane Pemphigoid
- Pemphigus Vulgaris
- Epithelial Dysplasia
- SCC
Considerations: OLP is potentially a premalignant lesion; lesions that do transform in SCC are observed to include both whitened tissue and erythema. The conversion rate is estimated to be 0.4-7.1% per year. Biopsy and long-term follow-ups should be performed to rule out malignancy and auto-immune disorders.
Conclusion
It is crucial to note that the clinical presentation of white lesions, oral epithelial dysplasia, and squamous cell carcinoma can vary. Therefore, it is crucial to establish a clear and definitive diagnosis. Regular check-ups and long-term follow-ups are essential, even throughout a person’s lifetime. In cases of uncertainty or suspicion of malignancy, performing biopsies and consulting an oral pathologist for evaluation becomes crucial. It can help prevent treatment delays, rule out malignancies in the early stage, and determine the most appropriate treatment approach for these lesions.
Postgraduate Oral Pathology and Radiology Certificate
Learn more about the clinical and didactic skills necessary to evaluate and manage patients with oral diseases by enrolling in Herman Ostrow School of USC’s online, competency-based certificate program in Oral Pathology and Radiology.
References
- 1) Brad W. Neville, DDS Distinguished University Professor Director, Division of Oral and Maxillofacial Pathology Department of Stomatology – Elsevier 3th.
- 2) https://emedicine.medscape.com/article/2105120-overview#showall
- 3) Mortazavi H, Safi Y, Baharvand M, Jafari S, Anbari F, Rahmani S. Oral White Lesions: An Updated Clinical Diagnostic Decision Tree. Dent J (Basel). 2019 Feb 7;7(1):15. doi: 10.3390/dj7010015. PMID: 30736423; PMCID: PMC6473409.
- 4) Brouns ER, Baart JA, Bloemena E, Karagozoglu H, van der Waal I. The relevance of uniform reporting in oral leukoplakia: definition, certainty factor and staging based on experience with 275 patients. Med Oral Patol Oral Cir Bucal. 2013 Jan 1;18(1):e19-26. doi: 10.4317/medoral.18756. PMID: 23085711; PMCID: PMC3548640.
- 5) Parlatescu I, Gheorghe C, Coculescu E, Tovaru S. Oral leukoplakia – an update. Maedica (Bucur). 2014 Mar;9(1):88-93. PMID: 25553134; PMCID: PMC4268300.

