Expertise can teleport. Metaphorically speaking. Technology is, however, reshaping healthcare and education, enabling expert knowledge and services to reach anyone, anywhere. In today’s rapidly evolving healthcare landscape, synchronous telemedicine, teledentistry, and tele-education are revolutionizing how healthcare and education are delivered, especially in rural and underserved communities. Digital solutions hold enormous potential to bridge the gap in healthcare access by providing remote consultations, health education, or workforce training. However, significant gaps still exist in regions, often due to limited infrastructure.
According to the Federal Communications Commission, 22.3% of rural Americans and 27.7% of those in Tribal lands lack access to fixed 25/3 Mbps broadband, compared to just 1.5% in urban areas. This connectivity gap severely hinders the effectiveness of telehealth solutions, preventing many individuals from accessing critical healthcare services and educational resources, which are crucial for improving health outcomes and achieving health education [1].
Without reliable internet access, many individuals in these communities cannot take full advantage of these transformative technologies. In such cases, public-private partnerships, including grant-funded programs, can support the expansion of broadband infrastructure and the necessary technology to reach underserved and vulnerable populations and those in need of health consultation and education via synchronous support. The implications are far-reaching for patients seeking medical and dental care and for the local workforce. Without proper training, an underprepared workforce may hinder efforts to improve overall population health and well-being.
Like what you’re learning? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Community Oral Health.
The rapid development of information and communication technology, particularly with the emergence of next-generation communication technologies like 5G and 6G, presents an incredible opportunity for the future of healthcare. As the global telemedicine market is projected to grow to $286.22 billion by 2030, telehealth adoption is no longer just a trend, it is a platform for population health [2].
Satellite technology, particularly the expansion of low-Earth orbit (LEO) satellite systems, offers an innovative solution to address this connectivity issue by providing internet access to remote areas that are otherwise difficult to serve using traditional broadband infrastructure [2]. Satellite networks can reach geographically isolated or challenging locations where building fiber-optic cables or cell towers is impractical. LEO satellite systems provided by companies specializing in space-based connectivity can drastically expand broadband access, enabling healthcare providers to deliver telehealth services and educational resources to areas underserved. However, the promise of satellite internet remains a proposal that has yet to be fully realized in terms of large-scale, impactful deployment in rural areas lacking broadband.
The success of telemedicine and tele-education services depends heavily on effective partnerships for funding, expertise, and disseminating their intended purpose. Public-private collaborations and grant funding may leverage satellite technology to deploy and integrate it into existing healthcare and education systems. Collaborations between government agencies, private companies, and healthcare institutions can bridge the digital divide for the remaining 25% of the U.S. population without broadband access.
Telehealth and tele-education services can also serve as intermediaries, providing remote consultations, health education, and training until in-person services are more accessible.
The Diffusion of Innovation Theory [3] illustrates into how new technologies can be adopted by populations to impact health outcomes. The theory posits that innovation adoption follows a pattern where early adopters, versus laggards, are proactive and inclined to adopt innovation (technology) within a community. Early adopters are typically more open to new ideas, willing to take risks, and often have decision-making discretion, allowing them to push the innovation forward within their communities. In the Community Oral Health Graduate Online certificate and master’s program, students learn practical applications of Diffusion of Innovation models.
Early adopters, particularly those in rural and underserved communities, could lead the charge in improving population health outcomes by addressing oral and general health issues; telehealth consults can lead to appropriate care plans [4]. However, the widespread success of such innovations depends on collaboration and public and private partnerships. For telehealth and tele-education to reach their full potential, organizations must create unified, collaborative efforts between local governments, private companies, and healthcare educators. Federal funding is a vital partnership for overcoming infrastructure challenges, enhancing care coordination and communication, and using telecommunication to reach vulnerable populations, as seen in Central California communities [5].
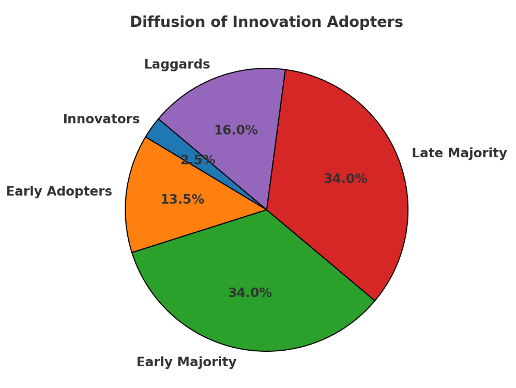
Figure 1 Diffusion of Innovation Adopters
As population health research continues to evolve, translating these advancements into scalable solutions requires alignment, readiness, and the establishment of practical innovation. Strong partnerships between the public and private sectors can help make these technologies more accessible, thus positioning providers and communities, particularly rural and underserved populations, to embrace telehealth and tele-education platforms that will ultimately improve their health and well-being [7]. Figure 1 illustrates innovation adoption on an S-curve, where the growth slows as most stakeholders have already adopted the innovation [6].
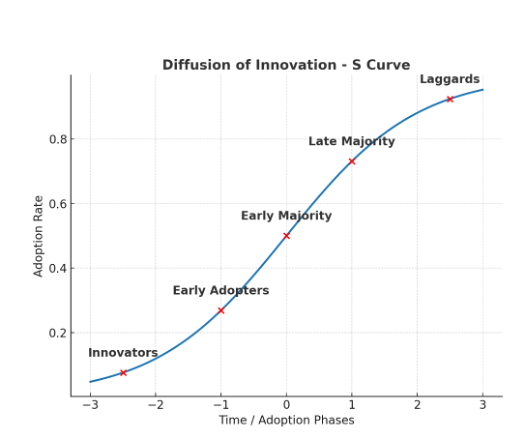
Figure 2 illustrates the five adopter groups emphasizing the smallest group, 2.5% and are the earliest to adopt innovation [6].
As population health research continues to evolve, translating these advancements into scalable solutions requires alignment, readiness, and the establishment of practical innovation. Strong partnerships between the public and private sectors can help make these technologies more accessible, thus positioning providers and communities, particularly rural and underserved populations, to embrace telehealth and tele-education platforms that will ultimately improve their health and well-being [7].
Earn an Online Postgraduate Degree in Community Oral Health
Do you like learning about a variety of issues while focused on the unique needs of community health dental programs? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Community Oral Health.
References
[1] U.S. Department of Agriculture USDA. Broadband. (n.d.). https://www.usda.gov/sustainability/infrastructure/broadband#:~:text=Reliable%20and%20affordable%20high%2Dspeed%20internet%20e%2DConnectivity%2C%20or,fundamental%20for%20economic%20activity%20throughout%20the%20US.&text=Unfortunately%2C%2022.3%20percent%20of%20Americans%20in%20rural,recent%20report%20by%20the%20Federal%20Communications%20Commission.
[2] D. Liu, S. Son, and J. Cao, “The determinants of public acceptance of telemedicine apps: an innovation diffusion perspective,” Frontiers in public health, vol. 11, pp. 1325031–1325031, 2023, doi: 10.3389/fpubh.2023.1325031.
[3] Y. Shaengchart and T. Kraiwanit, “Starlink satellite project impact on the Internet provider service in emerging economies,” Research in Globalization, vol. 6, pp. 100132-, 2023.
[4] Rural Health Information Hub. (n.d). Telehealth models for increasing access to specialty care. https://www.ruralhealthinfo.org/toolkits/telehealth/2/care-delivery/specialty-care#:~:text=Telehealth%20for%20Live%2Dvideo%20Teleconference,and%20reduce%20specialty%20care%20costs.
[5] U.S. Department of Health & Human Services HRSA. (2024). FY 2024:HRSA’s Rural Health Grants California fact sheet. https://www.hrsa.gov/sites/default/files/hrsa/rural-health/resources/fy-2024-california-fact-sheet.pdf
[6] Iqbal, M. & Zahidie, A. (2022) Diffusion of innovations: a guiding framework for public health. Scandinavian journal of public health. [Online] 50 (5), 533–537.
[7] X. Chen, K. Chen, M. Wang, and R. Li, “Roles of Wireless Networks in Bridging the Rural Smart Infrastructural Divide,” Infrastructures (Basel), vol. 8, no. 11, pp. 159-, 2023, doi: 10.3390/infrastructures8110159.