Osteonecrosis of the jaw (ONJ) occurs when there is damage to the bone that interrupts the nutrient supply or because of a medical condition that reduces bone health (Sedghizadeh, 2009). When the ONJ is associated with medications, it will be referred to as Medication-Related Osteonecrosis of the Jaw (MRONJ), which should be distinguished from other forms of ONJ and identified by the patient’s medical history and clinical exam (Ruggiero, 2022).
MRONJ manifests as a necrotic area in the jawbone exposed to the oral cavity, shows no signs of healing after at least 8 weeks of recognition or identification, and is not linked to previous or current radiation treatment. Recent evidence has indicated that MRONJ can be attributed to various antiresorptive agents extending beyond bisphosphonates, but also non-antiresorptive medications, including anti-angiogenic, tyrosine kinase inhibitors, and targeted therapies, including various chemotherapeutics and immunotherapeutics. Dental practitioners must know about these medications and recognize and provide appropriate management for patients at risk of developing MRONJ (Ruggiero, 2022).
Like what you’re learning? Download a brochure for our online, postgraduate Oral Pathology and Radiology certificate program.
New Drugs Associated with MRONJ
A study was conducted in the U.S. from 2010 to 2021, utilizing the FAERS (FDA Adverse Event Reporting System) database, a comprehensive collection of voluntarily reported adverse drug reactions (ADRs) associated with FDA-approved medications. The study identified 19,668 cases of medication-related jaw osteonecrosis (MRONJ) reported in the FAERS database from January 2010 to April 2021. Among the total cases, 8,908 met the inclusion criteria, being that 3,132 cases were reported from 2010 to 2014, and 5,776 cases were reported from 2015 to 2021 (Ahdi, 2023).
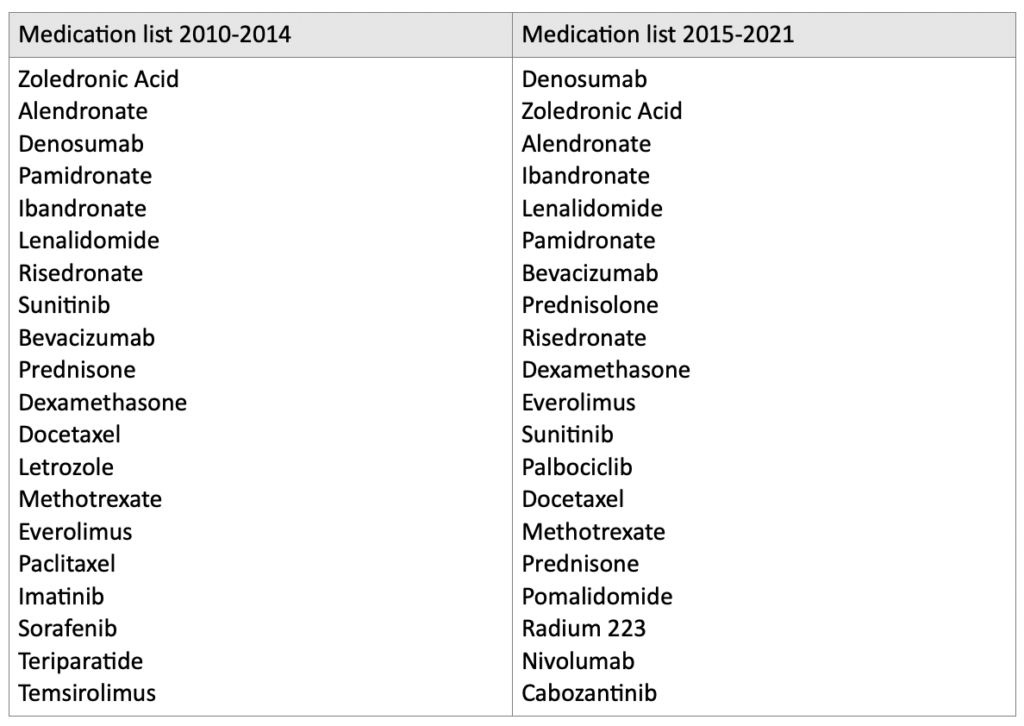
Upon reviewing the data from 2010 to 2014, several medications and drug classes associated with jaw osteonecrosis (ONJ) were identified. The drugs that had not been previously described include corticosteroids (prednisolone and dexamethasone), lenalidomide, docetaxel and paclitaxel, letrozole, methotrexate, imatinib, and teriparatide. New drugs and classes were also identified between 2015 and 2021, including palbociclib, pomalidomide, radium 223, nivolumab, and cabozantinib (Ahdi, 2023) (Table 1).
Table 1. Medication list of the twenty most commonly reported medications from 2010-2014 and from 2015-2021.
Considerations
According to the American Association of Oral and Maxillofacial Surgeons (AAOMS), the 2022 updated definition of medication-related osteonecrosis of the jaw (MRONJ) encompasses the following elements:
- Current or prior treatment with antiresorptive therapy alone or in combination with immune modulators or antiangiogenic medications. This includes medications such as bisphosphonates, denosumab, corticosteroids, and certain antiangiogenic agents.
- The presence of exposed bone or bone can be probed through an intraoral or extraoral fistula in the maxillofacial region, persisting for more than 8 weeks. This indicates the presence of non-healing bone in the jaw area.
- Absence of a history of radiation therapy to the jaws or metastatic disease in the jaws. These factors are excluded as potential causes for the observed osteonecrosis.
MRONJ Stage Classification
- STAGE 0: Patients in this stage show no clinical evidence of necrotic bone but may experience nonspecific symptoms. These symptoms can include odontalgia (tooth pain) that cannot be attributed to an odontogenic cause, dull and aching bone pain in the jaw that may radiate to the temporomandibular joint region, sinus pain accompanied by inflammation and thickening of the maxillary sinus wall and altered neurosensory function. Additionally, patients may exhibit tooth loosening that cannot be explained by chronic periodontal disease and may experience intraoral or extraoral swelling.
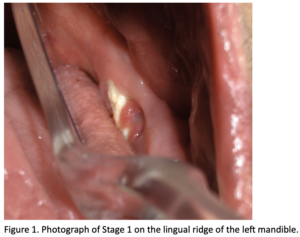
- STAGE 1: Exposed and necrotic bone or fistula that probes to the bone in asymptomatic patients with no evidence of infection/inflammation (Figure 1).
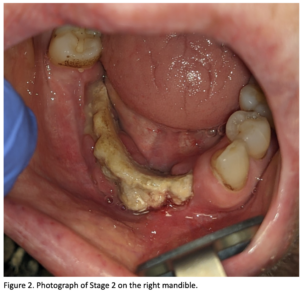
- STAGE 2: This stage of medication-related osteonecrosis of the jaw (MRONJ) is characterized by exposed and necrotic bone or a fistula that probes the bone. Patients in this stage are symptomatic and exhibit evidence of infection and inflammation (Figure 2).
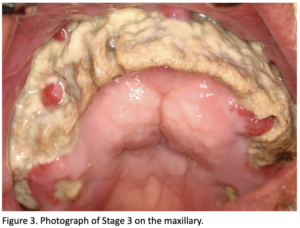
- STAGE 3: This stage is characterized by exposed and necrotic bone or fistulae that probe to the bone, with evidence of infection, and one or more of the following: exposed necrotic bone extending beyond the region of alveolar bone (i.e., inferior border and ramus in the mandible, maxillary sinus, and zygoma in the maxilla), pathologic fracture, extraoral fistula, oral antral/oral-nasal communication, osteolysis extending to the inferior border of the mandible or sinus floor (Ruggiero, 2022).
A recent study showed that medication-related jaw osteonecrosis (MRONJ) can be associated with many medications beyond bisphosphonates. While the antiresorptive drug group had the highest number of reported cases related to MRONJ, it is also important to consider the potential risks associated with other medications. Corticosteroids, such as prednisolone and dexamethasone, are commonly prescribed medications and can also contribute to the development of MRONJ. Additionally, other groups of medications, including immunomodulatory agents, tyrosine kinase inhibitors, immunosuppressives, and antineoplastic agents used in the treatment of various conditions, including neoplasia such as prostate, lung, breast cancer, and multiple myeloma, have been associated with MRONJ.
Local and systemic factors, patient habits, and overall health should also be considered as concomitant risk factors for the development of MRONJ. The presence of periodontal disease, inflammation, infection, innate or acquired immune disorders, and the lack of bone remodeling and angiogenesis can all play important roles in this condition.
Conclusion
It is crucial for clinicians and dental practitioners to be fully aware of the specific medications their patients are taking and to remain updated on advancements in drug therapies and their associated side effects, particularly those that can cause side effects in the oral cavity. Furthermore, many patients may need to be fully aware of the medications they are taking, or the specific risks associated with them.
This lack of awareness can pose difficulties for clinicians in accurately evaluating a patient’s medical history and developing suitable and safer treatment plans. Hence, we as dental clinicians must do a detailed evaluation of the patient’s medical history and embrace a proactively and multidisciplinary approach, if necessary, before any treatment decision to ensure reliable and effective treatment choices for our patients.
Postgraduate Oral Pathology and Radiology Certificate
Learn more about the clinical and didactic skills necessary to evaluate and manage patients with oral diseases by enrolling in Herman Ostrow School of USC’s online, competency-based certificate program in Oral Pathology and Radiology.
References
- Sedghizadeh, P. P. et al. (2009) Oral bisphosphonate use and the prevalence of osteonecrosis of the jaw: An institutional inquiry. The Journal of the American Dental Association (1939). [Online] 140 (1), 61–66.
- Ruggiero, S. L. et al. (2022) American Association of Oral and Maxillofacial Surgeons’ Position Paper on Medication-Related Osteonecrosis of the Jaws—2022 Update. Journal of oral and maxillofacial surgery. [Online] 80 (5), 920–943.
- Ahdi, H. S. et al. (2023) Medication-induced osteonecrosis of the jaw: a review of cases from the Food and Drug Administration Adverse Event Reporting System (FAERS). BMC pharmacology & toxicology. [Online] 24 (1), 15–15.



