April was Oral Cancer Awareness Month, a crucial time to highlight the importance of early detection and treatment of precancerous lesions in the mouth. What many people don’t realize is that most oral cancers begin as seemingly harmless changes in the mouth that are often painless and difficult to detect without professional examination. This blog is a collaborative effort during April’s Oral Cancer Awareness Month during USC’s Distance Learning Department outreach activities. This collaboration brings together emerging and established voices in dentistry to address the critical topic of oral pre-cancer detection.
Understanding Oral Pre-Cancer
Pre-cancer refers to abnormal cells in the mouth that have the potential to develop into cancer if left untreated. The World Health Organization (WHO) defines Oral Epithelial Dysplasia (OED) as a “spectrum of architectural and cytological cellular changes associated with an increased risk of progression to oral squamous cell carcinoma (OSCC)” [1].
The three most common types of pre-cancerous conditions seen in dental clinics are:
- Leukoplakia: “White plaque of questionable risk having excluded (other)known diseases or disorders that carry no increased risk of cancer”. Appears as a white patch that cannot be wiped (Figure 1) off and may become thicker over time. Often caused by irritation from smoking, rough teeth, or ill-fitting dentures. Risk of cancer development: 4-17% [2-7].
- Erythroplakia: Presents as a bright red, flat, and soft area in the mouth. Despite being less common than leukoplakia, it carries a much higher risk of malignant transformation (40-50%), even when small or seemingly harmless [2,3].
- Oral Lichen Planus: A chronic condition caused by an immune system reaction, typically appearing as white, lace-like patterns on both sides of the cheeks or tongue. Risk of cancer development: 0.4-6% [3,12].

Figure1. Leukoplakia (biopsy proven mild epithelial dysplasia) on the left lingual side of mandible.
Some patients may develop “speckled leukoplakia,” which combines white and red patches and carries an even higher risk of cancer development than either condition alone [3,6].
The Importance of Biopsy
Studies have shown that the rate of progression from oral leukoplakia to invasive cancer varies significantly, with reported rates ranging from 0% to 36%. Recent research indicates that OED and squamous cell carcinoma are present in approximately 40-46% of leukoplakia cases [6,7].
Due to this significant risk, oral health specialists often opt to perform a biopsy during the initial examination when suspicious lesions are found. This procedure involves removing a small piece of tissue under local anesthesia for oral pathology analysis to check for dysplasia or early cancer.
The American Dental Association recommends that any leukoplakia lesion showing signs of OED, regardless of severity, should be closely monitored for early indicators of malignant transformation [8].
Like what you’re learning? Download a brochure for our online, postgraduate Oral Pathology and Radiology certificate program.
Steps for Suspicious Lesions
When we find a suspicious lesion, several steps should be considered:
- Visual and tactile examination: We look at the shape, color, texture, and location of the lesion.
- Documentation: Taking clear photographs and notes helps in monitoring the lesion over time.
- Staining tests: Special dyes like toluidine blue or Lugol’s iodine can highlight abnormal areas that may not be obvious to the eye.
- Biopsy: This is the most important diagnostic tool. A small piece of tissue is removed under local anesthesia and sent to an oral pathology lab for histopathology assessment. The lab examines the cells for dysplasia or carcinoma in situ.
Based on the results, we can decide the next step in treatment. The key point is that early detection leads to better outcomes and less invasive treatments [9-12].
Clinical Decision-Making Process
When dealing with suspicious oral lesions, dental professionals follow a structured approach to diagnosis and treatment. The following flowchart (Figure 2) illustrates the typical decision-making process:
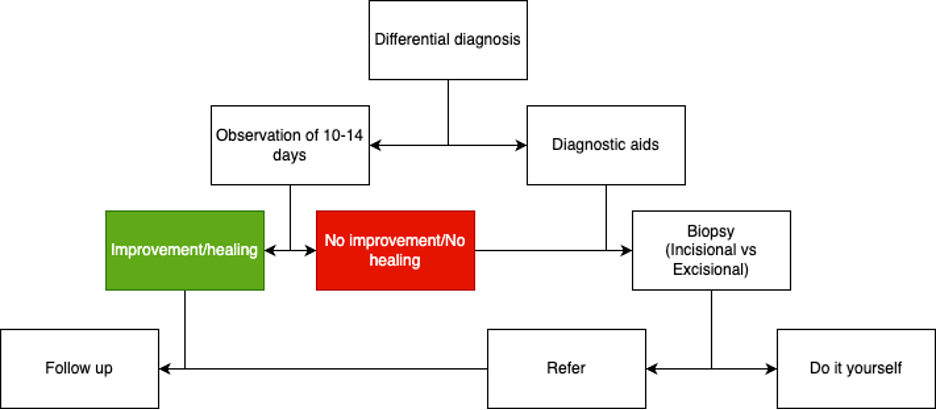
Figure 2. The following flowchart (Figure 2) illustrates the typical decision-making process with suspicious oral lesions. Starting with a differential diagnosis, clinicians typically:
- Observe the lesion for 10-14 days to monitor changes
- Use diagnostic aids for further assessment
- Perform a biopsy (incisional or excisional) if needed
- Based on results, either refer to specialists, provide follow-up care, or manage the condition directly
If improvement/healing occurs during the observation period, follow-up is recommended. If no improvement or healing is observed, a biopsy becomes necessary to rule out more serious conditions [8-12].
Treatment Options Based on Severity
Treatment decisions depend on several key factors:
- The severity of dysplasia
- Size and type of lesion
- Patient preferences
For mild dysplasia, a conservative “watch and wait” approach with regular follow-ups may be recommended. However, when mild dysplasia presents the features of proliferative verrucous leukoplakia ([PVL] a premalignant disorder which include a higher risk of malignancy) (Figure 3) or when moderate to severe dysplasia is found treatment intervention is recommended, which may include:
- Laser ablation
- Topical application of creams (e.g., off label use of imiquimod, 5-FU)
- Immunotherapy
- Surgical excision, among other that are in current research stages
The primary goal is to eliminate dysplastic tissue and reduce the risk of progression to cancer. The idea is to develop an individualized treatment plan based on the specific situation and risk profile for each patient [2-12].

Figure 3. Leukoplakia (biopsy proven mild epithelial dysplasia with PVL features) on the right side of hard palate.
Prevention and Risk Reduction
Understanding and reducing risk factors can help prevent pre-cancerous lesions from appearing or worsening [9,10]:
- Tobacco use: Both smoking and smokeless tobacco significantly increased risk
- Heavy alcohol consumption: Particularly when combined with tobacco use
- Chronic trauma: From ill-fitting dentures, rough fillings, or sharp teeth
- HPV infection: Especially relevant in younger patients
Preventive measures include:
- Quitting smoking and reducing alcohol consumption
- Maintaining excellent oral hygiene
- Addressing dental problems promptly
- Consuming a healthy, balanced diet
- Scheduling regular dental check-ups with oral cancer screenings
The Role of Dental Professionals
Dentists play a crucial role in the early detection of pre-cancerous lesions. During routine check-ups, they carefully examine the tongue, cheeks, gums, floor of the mouth, and palate for any abnormal changes.
Proper diagnosis and management of precancerous lesions is an extremely important responsibility of dental professionals. Regular intraoral examinations should be performed, and when suspicious lesions are detected, the diagnostic steps outlined above should be promptly utilized to make an accurate diagnosis [8-12].
Take Action
Don’t wait for symptoms to appear, by then, oral cancer may be in advanced stages. Schedule regular dental check-ups with your patients that include oral cancer screenings. If you notice any persistent changes in their mouth, such as white or red patches, sores that don’t heal within two weeks, or unexplained bleeding, consider biopsy or referral immediately.
Early detection of pre-cancerous lesions can prevent the development of oral cancer and potentially save life.
Postgraduate Oral Pathology and Radiology Certificate
Learn more about the clinical and didactic skills necessary to evaluate and manage patients with oral diseases by enrolling in Herman Ostrow School of USC’s online, competency-based certificate program in Oral Pathology and Radiology.
References
- Takata T, Slootweg P. Tumours of the oral cavity and mobile tongue: epithelial precursor lesions. In: El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ, eds. World Health Organization classification of Head and Neck Tumours. Lyon: IARC Press; 2017:112-114
- Mehanna HM, Rattay T, Smith J, McConkey CC. Treatment and follow-up of oral dysplasia-a systematic review and meta-analysis. Head Neck. 2009; 31(12):1600-1609.
- Warnakulasuriya S, Ariyawardana A. Malignant transformation of oral leukoplakia: a systematic review of observational studies. J Oral Pathol Med. 2016; 45(3):155-166.
- Lee JJ, Hong WK, Hittelman WN, et al. Predicting cancer development in oral leukoplakia: ten years of translational research. Clin Cancer Res. 2000;6(5): 1702-1710.
- William WN Jr, Papadimitrakopoulou V, Lee JJ, et al. Erlotinib and the risk of oral cancer: the Erlotinib Prevention of Oral Cancer (EPOC) randomized clinical trial. JAMA Oncol. 2016;2(2):209-216.
- Warnakulasuriya S, et al. (2016). “Oral epithelial dysplasia classification systems: predictive value, utility, weaknesses and scope for improvement.” Journal of Oral Pathology & Medicine, 45(6), 367-373.
- Petti S. (2003). “Pooled estimate of world leukoplakia prevalence: a systematic review.” Oral Oncology, 39(8), 770-780.
- Anil K Chaturvedi, Natalia Udaltsova, Eric A Engels, Jed A Katzel, Elizabeth L Yanik, Hormuzd A Katki, Mark W Lingen, Michael J Silverberg, Oral Leukoplakia and Risk of Progression to Oral Cancer: A Population-Based Cohort Study, JNCI: Journal of the National Cancer Institute, Volume 112, Issue 10, October 2020, Pages 1047-1054, https://doi.org/10.1093/jnci/djz238
- American Dental Association (ADA). “Oral Cancer Facts.” https://www.ada.org
- NHS. “Mouth cancer.” https://www.nhs.uk/conditions/mouth-cancer
- American Cancer Society. What are precancers and precancerous cells. https://www.cancer.org/cancer/understanding-cancer/what-is-cancer/precancer.html
- Tilakaratne WM, Jayasooriya PR, Jayasuriya NS, De Silva RK. Oral epithelial dysplasia: Causes, quantification, prognosis, and management challenges. Periodontol 2000. 2019 Jun;80(1):126-147.





