Dr. Glenn Clark, DDS developed this content for his Systems Physiology, Sleep, Motor Disorders Course for Dental Residents of the Orofacial Pain and Oral Medicine master’s program at the Herman Ostrow School of Dentistry of USC.
Why is sleep a concern for dentists?
The story of dentists and sleep begins with Dr. Pierre Robin. Dr. Robin is famous for describing children born with a mandibular growth insufficiency, which is now known as Pierre Robin Syndrome (PRS). Dr. Robin also coined the term Glossoptosis, which means the abnormal downward or back placement of the tongue, and published his first article on this in 1923.
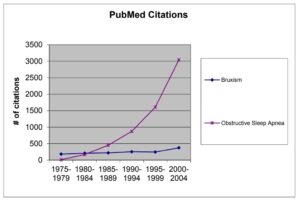
Dentists have always been interested in sleep because of bruxism, or the grinding of teeth, which sometimes is a powerful destructive motor event occurring during sleep. The field of sleep disorders is relatively new. With new scientific discoveries, we understand better the critical role the tongue and the jaw play in causing and preventing sleep-disordered breathing.
The graph below shows growth of the number of citations in Medline in the topic of bruxism (which is not growing) and Obstructive Sleep Apnea which exhibits rapid, maybe even exponential growth.
Like what you’re learning? Take it a step further and test your clinical diagnosis skills with USC’s Virtual Patient Simulation. Review real-life patient histories, symptoms, and imaging, conduct a medical interview and clinical exam, make a diagnosis, and create a treatment plan for virtual patients experiencing Orofacial Pain conditions.

The disorders of sleep are multiple, and they are categorized by The International Classification of Sleep Disorders (ICD-9-CM). The various disorders which are cataloged by this system are presented below. In 2005, an update of this classification was published.
If you are wondering why you should review this list of diseases, it is necessary to know a little about these other problems if patients with a possible Sleep-Breathing Disorder.
Sleep-Disordered Breathing
Why do people wake up in the middle of the night?
Many reasons exist for this including urination urges, loss of slow-wave sleep as we age, the natural cycling of sleep from deep to shallow and back again, anxiety and worries that creep into our subconsciousness during sleep.1
One interesting fact about sleep is that as we age, we sleep less, “From midlife until the eighth decade, total sleep time decreased, on average, by 27 minutes per decade.” What is evident is that by about 60, we sleep on average, only 5 hours.
Classification of Sleep Disorders
The International Classification of Sleep Disorders has published a list of sleep disorders, and it has been updated several times since it was first published in 1990 (i.e., 1990, 1997, 2001, 2005).
ICSD-2 Sleep Disorder Categories
- Insomnias
- Sleep-related breathing disorders
- Hypersomnias of central origin
- Circadian rhythm sleep disorders
- Parasomnias
- Sleep-related movement disorders
- Isolated symptoms, apparently normal variants and unresolved issues
- Other sleep disorders
ICD-9 & ICD-10 Sleep-Related Breathing Disorders
| Sleep-Related Breathing Disorders | (ICD-9) | (ICD-10) |
| Obstructive sleep apnea, adult | 327.23 | G47.33 |
| Obstructive sleep apnea, pediatric | 327.23 | G47.33 |
| Sleep apnea/sleep related breathing disorder, unspecified | 320.2 | G47.30 |
| Restless legs syndrome | 333.49 | G25.81 |
| Periodic limb movement disorder | 327.51 | G47.61 |
| Sleep-related leg cramps | 327.52 | G47.62 |
| Sleep-related bruxism | 327.53 | G47.63 |
| Sleep-related rhythmic movement disorder | 327.59 | G47.69 |
| Sleep-related movement disorder (NOS) | 327.59 | G47.90 |
| Sleep-related movement disorder due to drug or substance | 327.59 | G47.67 |
| Sleep-related movement disorder due to medical condition | 327.59 | G47.67 |
What are Circadian Rhythm Sleep Disorders?
Circadian Rhythm Sleep Disorders are related to the timing of sleep within the 24-hour day. Some of these disorders are influenced by the timing of the sleep period that is under the individual’s control (e.g., shift work or time-zone change). Other disorders are influenced by neurologic mechanisms (e.g., irregular sleep-wake pattern and advanced sleep-phase syndrome). Although some of these disorders can be present in both an intrinsic and extrinsic forms, their common linkage through chronobiologic, pathophysiologic mechanisms determines their recognition as a homogeneous group of disorders.
What are parasomnias?
Parasomnias are disorders of arousal, partial arousal, and sleep-stage transition. While there are many causes of involuntary motor activity in the jaw, if they occur during sleep, they are called parasomnias. Parasomnias include talking, repeated jaw motions such as chewing or grinding and occasional a rapid closure of the jaw.
The snapping shut motion of the jaw or repeated twitching of the palate is called myoclonus. The definition of myoclonus is a sudden, brief, shock-like, involuntary movements caused by muscular contractions.2 Myoclonus therapy is limited and usually involves symptomatic treatment with valproic acid or clonazepam.
4 Types of Parasomnias
Parasomnias are problems that intrude into the sleep process and are not primarily disorders of sleep or wake states. These disorders, which are four in number, are manifestations of central nervous system activation, usually transmitted through the skeletal muscle or the autonomic nervous system.
1. Arousal Disorders
Arousal disorders are manifestations of partial arousal that occur during sleep. These disorders are the “classic” arousal disorders that appear to be primarily disorders of normal arousal mechanisms.
2. Sleep-Wake Transition Disorders
Sleep-wake transition disorders occur mainly during the transition from wakefulness to sleep or from one sleep stage to another. Under some circumstances these disorders can occur within specific sleep stages, but it is usually the exception rather than the rule.
3. Parasomnias Associated with REM Sleep
The parasomnias usually associated with REM sleep have their onset during the REM sleep stage; some of these REM sleep parasomnias do occur during other sleep stages, but this occurrence is rare.
4. Other Parasomnias
Other parasomnias are those parasomnias that do not fall into the categories of arousal disorders, sleep-wake transition disorders, or parasomnias associated with REM sleep.
What is Obstructive Sleep Apnea?
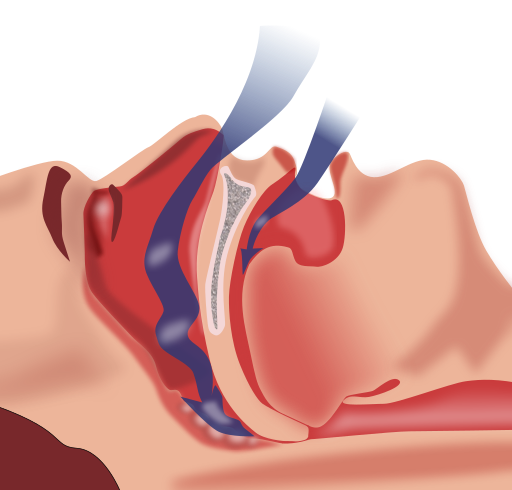
Obstructive Sleep Apnea (OSA) is the episodic closure of the airway when the muscles of the body relax during sleep. Mild OSA occurs in 20% adults and 7% have moderate OSA.3 A 2006 study found 31% of men and 21% of women in the USA are at a high risk of OSA.4
Unresolved moderate to severe OSA can lead to increased cardiovascular disease and cognitive deterioration. Dentists caring for adults with OSA should consult the American Academy of Sleep Medicine’s guidelines for the long-term care of obstructive sleep apnea.
What is Central Sleep Apnea?
Central Sleep Apnea (CSA) is the failure to breathe that occurs when the brain’s respiratory control center momentarily shuts down during sleep, fails to signal the respiratory system to breathe in, and causes the individual to miss one or more respiratory cycles.5
Obstructive Sleep Apnea Workup
Do you suspect a new patient of sleep-disordered breathing? Conduct a workup for obstructive sleep apnea. The workup should include:
- Interviewing the patient’s bed partner,
- Gathering information regarding regular episodes of excessive daytime sleepiness,
- Completing a physical and TMD examination
- Identifying if the patient is at high risk for a cardiovascular event
Mandibular Advancement Devices
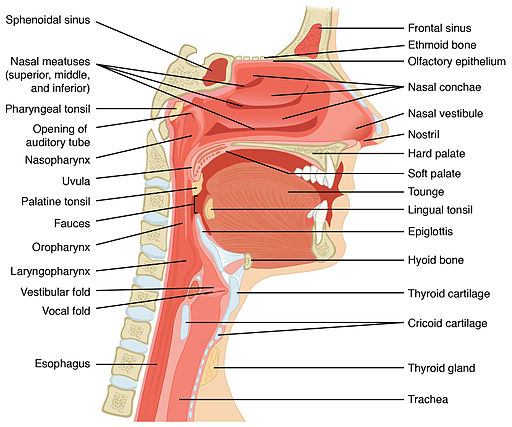
The most common reason you would complete a full dental and Temporomandibular Disorder (TMD) exam is to see if the patient would benefit from a Mandibular Advancement Device (MAD). MADs can help patients with Obstructive Sleep Apnea decrease snoring by moving the jaw forward, thereby increasing the size of the upper airway and reducing restriction in the back of the throat.7
Sleep Apnea Questionnaires
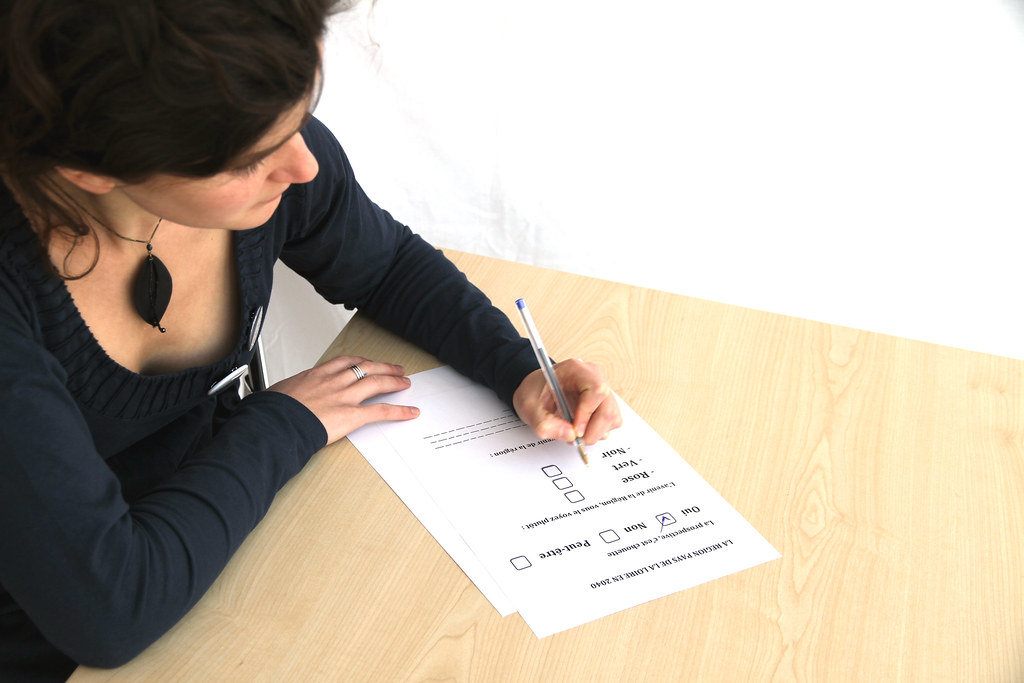
When dentists need to test for hypersomnolence or Obstructive Sleep Apnea, questionnaires related to sleep can be helpful.
1. Modified Berlin Questionnaire
When used in conjunction with a patient’s BMI score, the Modified Berlin Questionnaire is a good predictor of Obstructive Sleep Apnea risk. The Modified Berlin Questionnaire asks questions related to snoring and breathing difficulties.
2. Epworth Sleepiness Questionnaire
The Epworth Sleepiness Scale (ESS) indicates sleepiness by gauging how likely are you to fall asleep while performing activities like sitting, reading, and watching TV.
3. Multiple Sleep Latency (MSL) Test
The Multiple Sleep Latency Test measure how long it takes someone to fall asleep. It works under the presumption that the more tired a person is, the quicker they will fall asleep. Epworth Sleepiness Scale cannot replace Multiple Sleep Latency test.6
Sleep Apnea Dental Exam

This 14-step process is covered in full detail in our comprehensive Obstructive Sleep Apnea dental exam article, and dentists should complete this physical examination when assessing a possible OSA patient.
- Measure the jaw opening
- Measure the lateral and protrusion motion of the jaw
- Auscultation of temporomandibular joints for sounds
- Test Masticatory Muscle Tenderness
- Test temporomandibular joint Palpation for Tenderness
- Examine anterior teeth for attrition
- Examine the mucosal tissue
- Test for occlusal stability
- Inspect for periodontal diseases, caries, and local disease
- Test for nasal airway obstruction
- Examine Palate/Uvula length and inflammation
- Rule out enlarged tonsils
- Rule out substantial Micrognathia
- Rule out an excessively large tongue
Imaging Obstructive Sleep Apnea
To diagnose a new patient, a dentist might consider imaging the site of obstruction for OSA. However, imaging the airway with a CT Scan or an Ultrafast MRI to predict OSA is not effective. MRIs are often too loud for patients to fall asleep, and while researchers generally found a difference in airway size using CT scans, the differences are lost when you match OSA and Non-OSA patients by weight and age.
Snoring Disorders
Snoring is characterized by loud upper airway (back of the mouth, nose, and throat) breathing sounds in sleep, without episodes of sleep apnea or hypoventilation, and it affects approximately 30% of the adult population over 30 years of age. While snoring disorders are generally perceived as a social nuisance, it can lead to OSA syndrome.
3 Types of Snoring
1. Palatal Flutter Sounds
Palatal flutter sounds are typically produced by the vibration of pharyngeal tissues (posterior base of the tongue, soft palate, uvula, posterior pharyngeal wall) due to turbulent airflow through a narrow oropharyngeal.
2. Nasal Snoring
Non-palatal snoring is less common, and is typically understood as nasal tissue vibration originating from the retroglossal or hypoglossal region of the throat; specifically the epiglottis, hypopharyngeal, and tongue base area.
3. Retroglossal, Epiglottal, and Hypoglossal Snoring
Palatal snoring produces explosive peaks of sound at low frequency (below approximately 100 Hz). In contrast, non-palatal snorers produced a higher frequency snoring sound.
Measuring the acoustic characteristics of snoring might be a better diagnostic method than nasal endoscopy since the frequency of snoring sounds predict the site of the recording.
Earn an Online Postgraduate Degree in Orofacial Pain and Oral Medicine
Are you interested in a variety of issues focused on orofacial pain, medicine and sleep disorders? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Orofacial Pain and Oral Medicine.

