So we talked about traumatic ulcerations we talked about squamous cell carcinoma, and OPSCC and HPV. Now we’re going to talk about infectious ulcerative lesions including Histoplasmosis and Mucurmycosis.
If you’re looking for a clinical test to confirm a fungal infection in one of your patients, please consider reading our article, How to Perform an Agar Slant Culture Test for Fungal Infections.
Don’t have time to read this article? We get it. Download the Diagnosing Vesicular Ulcerative Conditions checklist to get all the key information and images from this article plus all the other conditions we cover in the Dentist’s Guide to Oral Pathology.

Infectious Ulcerative Lesions

When you see something like this: very large ulcerative lesion that looks necrotic, hemorrhagic, irregular, granulomatous, you have to think of squamous cell carcinoma. Squamous cell carcinoma should be number one on your differential.
Trauma not so much because it’s diffusely involved compared to the first example of traumatic loss around the tongue. Trauma should be on your differential if it is a smaller lesion, and then you have to include deep fungal infection and TB.
This was not painful surprisingly. With trauma you would think something would be painful. Cancer, unless it’s very advanced, is not painful. This would be very concerning. The top of my differential would be squamous cell carcinoma here. Also, metastatic disease and lymphoma can’t be excluded.
Histoplasmosis Histology
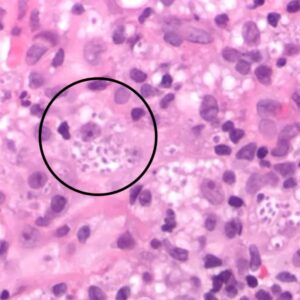
We took a biopsy and lo and behold we saw no cancer. We saw these large histiocytic cells. When we looked really closely we saw these little, round things. We weren’t sure what they were. This can look just like karyorrhexis. Specifically, when there’s a lot of inflammation, more so when there’s lots of plasma cells, the cell is going to fall apart. Because they’re dying, this can look like cellular debris.
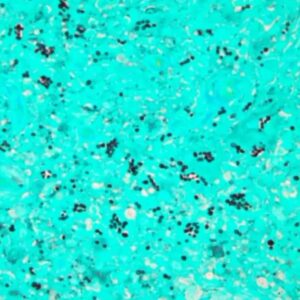
We did a GMS stain and it turned out that those little round spots were a fungal organism. You can see all these organisms being highlighted in the corresponding PAS stain. Because the microorganisms are so small this example of a deep fungal infection can be easily overlooked.
Histoplasmosis Clinical Features
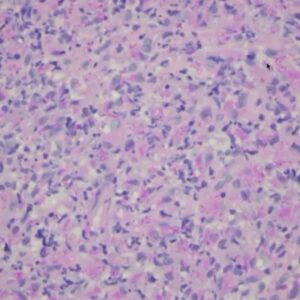
Histoplasmosis or H. capsulatum or dimorphic fungus, is the most common deep fungal infection and commonly will present in the oral cavity as an indurated ulceration. It’s kind of like what we we saw on the gingiva, but sometimes it can look just like squamous cell carcinoma bilateral tongue or traumatic ulcer of the lateral tongue.
The primary infection is pulmonary. If you see it in the oral cavity that means that it has already disseminated and that it needs to be promptly addressed. If a deep fungal infection is disseminated, patients are at risk for adrenal failure and death.
Histoplasmosis Diagnosis and Treatment
Histoplasmosis is an infection that’s usually inhaled by spores and typically found in specific regions of the United States and other areas. The diagnosis is typically made by biopsy and then confirmed by an agar slant culture test or urine test. The treatment is heavy, systemic anti-fungal agents such as Amorphotericin B or Itraconazole.



Images Courtesy of Indraneel Bhattacharyya from UF Oral Pathology
- Zoster-related sores
- Oral ulceration of a deep fungal infection. You can see inner necrotic area in the center. This is histoplasmosis.
- This is histoplasmosis. Squamous cell carcinoma of the dorsal tongue is very rare. Take a biopsy here, lesion and all.
Geographic Distribution of Deep Fungal Infections
There are other types of deep fungal infections namely Blastomycosis and Coccidioidomycosis. This is the greographic distribution of endemic fungal infections.
Histoplasmosis is limited to Ohio and the Mississippi River Valley. I diagnosed a case last year in California so it’s not limited, just most common. Coccidioidomycosis is found in the southwestern USA, Mexico, and the San Joaquin Valley area. Blastomycosis is local to the Great Lakes area. Blastomycosis is usually found in soil that’s disrupted and sometimes in bat droppings.

Mucormycosis Symptoms


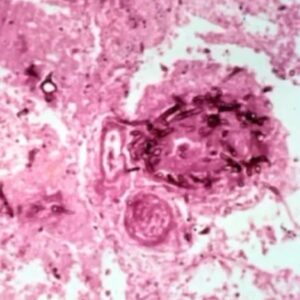
This patient had uncontrolled diabetes. My mentor saw this patient on her rounds in the hospital. They took a look and it didn’t look good. When they touched the area it just fell apart. This was all necrotic bone and necrotic tissue.
They took a biopsy and revealed very sparse fungal organisms and mostly necrosis. This can be easily overlooked. Without a stain it can be very difficult to see. This is mucormycosis, and if you do a stain you can see the organisms a better. Mucormycosis is invasive so it’s going into the blood vessels and causing lots of necrosis. This is an emergency.
Mucormycosis Diagnosis
This all occurred before the diagnosis was given and the patient passed away. These patients don’t fare well. About 60% of patients that suffer from Mucormycosis will die. It’s usually seen in the setting of uncontrolled diabetes. A biopsy is necessary for specific diagnosis.

This is one patient that actually survived Mucormycosis and was left with a large defect. Patients do survive and when they do they are usually left with an oroantral fistula. When you see this you have to think of other differentials.
Differential Midline Ulcerations
- Extranodal NK/T cell lymphoma, nasal type
- NUT midline carcinoma, nasal carcinoma
- Mucormycosis, an invasive fungal sinusitis
- Tertiary syphilis
- Wegener granulomatosis
- Salivary gland malignancy
- Cocaine abuse
All of these can cause this type of appearance. Necrosis is secondary to cocaine which is a vasoconstrictor. So these are your differentials for midline ulcerations.
Postgraduate Oral Pathology and Radiology Certificate
Learn more about the clinical and didactic skills necessary to evaluate and manage patients with oral diseases by enrolling in Herman Ostrow School of USC’s online, competency-based certificate program in Oral Pathology and Radiology.

