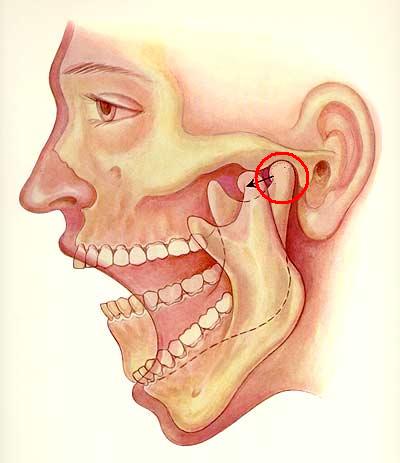
The temporomandibular joint (TMJ) comprises the mandibular condyle and the glenoid fossa of the temporal bone, covered by fibrocartilage, which provides greater resilience and support to mechanical stress [1]. This joint can be affected by bone deterioration, causing impaired TMJ function and leading to the diagnosis of TMJ Osteoarthritis (TMJ-OA). Similar to other joints, TMJ-OA causes a gradual breakdown of cartilage, sclerosis in the subchondral bone, and the emergence of osteophytes [2]. TMJ-OA presents unique challenges, particularly for young people, where the symptoms often progress without significant inflammatory symptoms, making early diagnosis and intervention challenging [3,4]
Etiology & Pathophysiology
Osteoarthritis (OA) is a degenerative joint disease marked by cartilage degeneration, bone sclerosis, and osteophyte formation. Its onset is influenced by various local and systemic factors, making it a multifactorial disease [4]. Degenerative changes in the TMJ stem from an imbalance between joint loading and its capacity for adaptation, involving dynamic processes and structural flexibility. Stressors and long-term habits such as clenching and grinding teeth, and other bad habits such as biting nails and biting pencils, among others, contribute to acting at the molecular level and can disrupt this balance, culminating in functional disorders observed during clinical examinations [5].
Like what you’re learning? Download a brochure for our Orofacial Pain and Oral Medicine certificate or master’s degree program in partnership with the Keck School of Medicine of USC.
Diagnosis
The diagnosis of OA involves a comprehensive approach, including medical history, clinical examination, and radiological examinations (imaging will show degenerative joint changes in several degrees, most commonly seen in the condylar head). Typical clinical findings include joint pain (arthralgia unilateral or bilateral) exacerbated during jaw movements, jaw movement limitations, bite changes (new onset of occlusal changes), and crepitus ( or crunching noises) [6]. Imaging modalities like computed tomography (CT) and cone beam computed tomography (CBCT) offer detailed visualization of bone structures, while magnetic resonance imaging (MRI) is crucial for articular disc position assessment [1]. Conventional radiographs, such as a panoramic radiograph, may reveal advanced bone destruction, aiding a first approach for TMJ assessment a 3D imaging as the CBCT for assessing OA severity is recommended for definitive details of this condition, which typically presents with osteophytes, erosion, and subcortical pseudocysts [7]. However, diagnosing OA remains challenging due to the weak correlation between symptom severity and radiographic findings [6].
Treatment Treatment for TMJ-OA can be categorized into non-invasive and invasive approaches [4]. Non-invasive options involve patient education in a home rehabilitation program, including but not limited to TMJ hinge exercises, avoidance protocol for bad habits that can harm the TMJ functionality, such as clenching (practicing N-position), nightguard or interocclusal appliances, with NSAIDs being the most common pain-relief medication [4]. Although they don’t directly address OA, splints can mitigate joint stress factors. Minimally invasive procedures encompass TMJ joint injection with corticosteroid and local anesthetic, as well as arthrocentesis with hyaluronic acid, which have been shown as one of the treatment options [4]. Surgical intervention, while less common, is reserved for non-responsive cases. However, evidence supporting the efficacy of invasive methods in TMJ treatment remains limited [4].
Osteoarthritis and Age
Numerous studies have established a correlation between osteoarthritis (OA) frequency and progression and aging. This relationship is attributed to the TMJ’s exposure to various biological changes associated with advancing age [2]. As individuals age, there is an increase in the calcium content within the articular disk, rendering it stronger yet less elastic and more susceptible to strain [4]. While it is true that age is a significant risk factor for developing osteoarthritis, it is by no means the sole determinant, especially in the case of TMJ-OA. Interestingly, severe cases of TMJ-OA can manifest in younger patients [4]. Many of these patients have a history of long-term clenching habits, autoimmune diseases (more commonly seen in rheumatoid diseases), and/or a history of trauma, suggesting a potential contributing factor, as these injuries can disrupt the normal functioning of the joints and accelerate the degenerative process, leading to the premature onset of osteoarthritis [4,8,9].
Genetics also may play a significant role in determining an individual’s risk of developing osteoarthritis. Certain genetic factors can predispose individuals to cartilage degeneration and joint abnormalities, making them more susceptible to developing OA at a younger age [10,11]. Family history of the condition can be a strong indicator of one’s likelihood of developing OA, even in the absence of other risk factors. Additionally, hormonal imbalances may exacerbate or trigger TMJ-OA in younger populations, particularly among women. Hormonal fluctuations, particularly during childbearing years, may exacerbate facial pain, and decreased estrogen levels during menopause can lead to TMJ degeneration and increased alveolar bone loss [12]. These factors potentially implicate the role of estrogen signaling in the development and/or exacerbation of TMJ-OA.
Conclusion
The prevalence of TMJ-OA in younger populations highlights a crucial public health concern that merits attention. While advancing age is indeed a significant risk factor, it is not the only factor at play when it comes to TMJ-OA. Younger individuals can develop TMJ-OA due to a variety of reasons, including but not limited to genetic predisposition, hormonal influence, and aggravated trauma and mechanical stress.
Earn an Online Postgraduate Degree in Orofacial Pain and Oral Medicine
Like what you’re learning? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Orofacial Pain and Oral Medicine in partnership with the Keck School of Medicine of USC.
References
- Ahmad M, Schiffman EL. Temporomandibular Joint Disorders and Orofacial Pain. Dent Clin North Am. 2016 Jan;60(1):105-24. doi: 10.1016/j.cden.2015.08.004. Epub 2015 Oct 21. PMID: 26614951; PMCID: PMC6762033.
- M. Kalladka, S. Quek, G. Heir, E. Eliav, M. Mupparapu, A. Viswanath, Temporomandibular Joint Osteoarthritis: Diagnosis and Long-Term Conservative Management: A Topic Review, J Indian Prosthodont Soc 14 (2014) 6–15. https://doi.org/10.1007/s13191-013-0321-3
- V. Gandhi, G. Sharma, E.H. Dutra, P.-J. Chen, S. Yadav, Degenerative disorder of temporomandibular joint- current practices and treatment modality, Seminars in Orthodontics (2023). https://doi.org/10.1053/j.sodo.2023.12.007
- Tanaka E, Detamore MS, Mercuri LG. Degenerative disorders of the temporomandibular joint: etiology, diagnosis, and treatment. J Dent Res. 2008 Apr;87(4):296-307. doi: 10.1177/154405910808700406. PMID: 18362309.
- S.B. Milam, Pathogenesis of degenerative temporomandibular joint arthritides, Odontology 93 (2005) 7–15. https://doi.org/10.1007/s10266-005-0056-7
- R. Poveda Roda, J.M. Díaz Fernández, S. Hernández Bazán, Y. Jiménez Soriano, M. Margaix, G. Sarrión, A review of temporomandibular joint disease (TMJD). Part II: Clinical and radiological semiology. Morbidity processes, Med Oral Patol Oral Cir Bucal 13 (2008) E102-109.
- Plesh O, Adams SH, Gansky SA. Temporomandibular joint and muscle disorder-type pain and comorbid pains in a national US sample. J Orofac Pain. 2011 Summer;25(3):190-8. PMID: 21837286; PMCID: PMC3807573.
- Yun PY, Kim YK. The role of facial trauma as a possible etiologic factor in temporomandibular joint disorder. J Oral Maxillofac Surg. 2005 Nov;63(11):1576-83. doi: 10.1016/j.joms.2005.05.318. PMID: 16243173.
- Shoohanizad E, Garajei A, Enamzadeh A, Yari A. Nonsurgical management of temporomandibular joint autoimmune disorders. AIMS Public Health. 2019 Dec 12;6(4):554-567. doi: 10.3934/publichealth.2019.4.554. PMID: 31909075; PMCID: PMC6940567.
- J.-H. Kang, Transcriptomes in peripheral blood of young females with temporomandibular joint osteoarthritis, Sci Rep 11 (2021) 8872. https://doi.org/10.1038/s41598-021-88275-8
- D. Sangani, A. Suzuki, H. VonVille, J.E. Hixson, J. Iwata, Gene Mutations Associated with Temporomandibular Joint Disorders: A Systematic Review, OAlib 2 (2015) e1583. https://doi.org/10.4236/oalib.1101583
- J.L. Robinson, P.M. Johnson, K. Kister, M.T. Yin, J. Chen, S. Wadhwa, Estrogen signaling impacts temporomandibular joint and periodontal disease pathology, Odontology 108 (2020) 153–165. https://doi.org/10.1007/s10266-019-00439-1

