Your mouth is one of your body’s most important warning systems. Tongue lesions may indicate a local disease process or an overall systemic issue. Approximately 15.5 percent of US adults present with tongue lesions according to the National Health and Nutrition Examination Survey. This percentage increases with tobacco use and if an individual wears dentures. It is important that everyone is comfortable doing a tongue evaluation on themselves. After you do it once or twice, you will see how quickly it can be done.
How to Evaluate Your Own Tongue?
In between dental visits, it is important to evaluate your tongue for any changes. This is easily done in four steps:
- Look at the top of your tongue for any new areas of discoloration or growths.
- Use the back end of your toothbrush to gently depress the center of your tongue and say Ahh- evaluate the back of your tongue near your throat.
- Use a clean facecloth to gently grab the tip of your tongue and pull it gently out and to each side. Look at the side border of the tongue for any changes.
- Lift up your tongue to the roof of your mouth so that you can visualize the under-surface of your tongue. Also, use this opportunity to evaluate the floor of your mouth.
- If you see anything unusual or if you have new and unexplained pain and or symptoms, contact your dentist for an evaluation.
Like what you’re learning? Download a brochure for our online, postgraduate Oral Pathology and Radiology certificate program.
Here are some common tongue conditions:
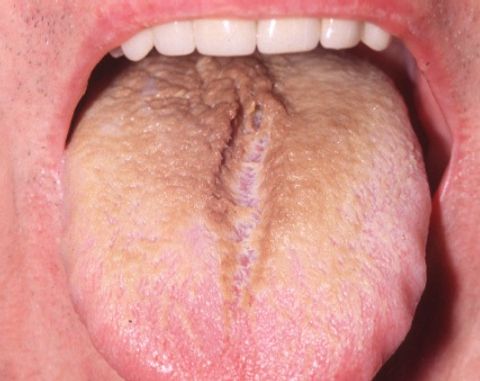
Median Rhomboid Glossitis
Presents as a smooth shiny lesion in the central part of the tongue. May be asymptomatic but patients can have a burning or itching sensation. A yeast infection is thought to be the cause of this condition.

Benign Migratory Glossitis
Also known as geographic tongue. Is an inflammatory condition characterized by alternating raised plaques and smooth, atrophic areas. The lesions are “migratory” and can change over hours. Etiology is unknown but an association with psoriasis has been found.

Atrophic Glossitis
Presents as a smooth or glossy appearance partially or throughout the dorsum of the tongue. Typically due to a nutritional deficiency or an underlying disease or medication use.

Photo courtesy of Gupta, Shreya et al. “Atrophic Glossitis: Burning Agony of Nutritional Deficiency Anemia.” (2017).
Hairy Tongue
Benign condition with obvious discoloration (black, tan, white) on the dorsum of the tongue. Can be caused by smoking, xerostomia, poor oral hygiene, excessive coffee/tea consumption, and medications. Treatment involves discontinuation of the responsible agent and/or gentle tongue scraping.
Oral Hairy Leukoplakia
Commonly presents as a white, asymptomatic, corrugated plaque on the lateral border of the tongue that does not rub off. Is an Epstein Barr infection found in immunocompromised individuals especially those with concomitant HIV infection?
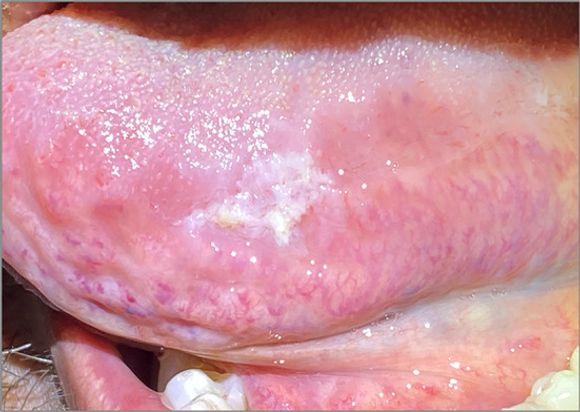
Leukoplakia
Adherent white patch found anywhere in the mouth but commonly found on the tongue and the floor of the mouth. Strongly associated with tobacco use but not necessary to occur. A biopsy is necessary to rule out a malignancy.

Squamous Cell Carcinoma
The most common oral malignancy. Can have a varied presentation: patch, nodule, or ulcer. Can be red or white or a mixture of both. Found most commonly are the lateral and ventral surfaces of the tongue as well as the floor of the mouth. A biopsy is indicated as soon as a lesion is identified.

Postgraduate Oral Pathology and Radiology Certificate
Learn more about the clinical and didactic skills necessary to evaluate and manage patients with oral diseases by enrolling in Herman Ostrow School of USC’s online, competency-based certificate program in Oral Pathology and Radiology.
References
- Reamy BV, Derby R, Bunt CW. Common tongue conditions in primary care. Am Fam Physician. 2010 Mar 1;81(5):627-34. PMID: 20187599.
- Gupta, Shreya et al. “Atrophic Glossitis: Burning Agony of Nutritional Deficiency Anemia.” (2017).
- Gurvits GE, Tan A. Black hairy tongue syndrome. World J Gastroenterol. 2014 Aug 21;20(31):10845-50. doi: 10.3748/wjg.v20.i31.10845. PMID: 25152586; PMCID: PMC4138463.
- Alramadhan SA, Bhattacharyya I, Cohen DM, Islam MN. Oral Hairy Leukoplakia in Immunocompetent Patients Revisited with Literature Review. Head Neck Pathol. 2021 Sep;15(3):989-993. doi: 10.1007/s12105-021-01287-8. Epub 2021 Jan 11. PMID: 33428065; PMCID: PMC8384929.
- Mangold AR, Torgerson RR, Rogers RS 3rd. Diseases of the tongue. Clin Dermatol. 2016 Jul-Aug;34(4):458-69. doi: 10.1016/j.clindermatol.2016.02.018. Epub 2016 Mar 8. PMID: 27343960

