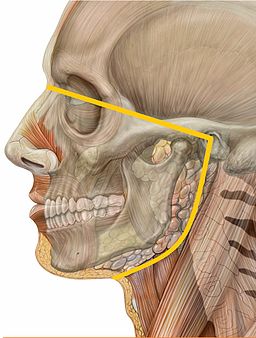
This blog is step 4 of Dr. Glenn Clark’s 5-step process for diagnosing Chronic Trigeminal Neuralgia. Dr. Clark, Director of USC’s Online Master’s Degree in Orofacial Pain and Oral Medicine teaches dental residents how to diagnose neuropathic pain from nociceptive.
By now you should have ruled out local pathology, tested for pulp vitality, and ruled out tooth fractures as the source of pain.
The problem is nociceptive and neuropathic pains both cause pain so how are they distinguished. Well, one way is too collect more information about the onset, character, severity, duration, pattern and location of the pain.
Distinguishing between nociceptive and neuropathic pain can be done with a thorough set of interview questions, and it can be supplemented with a pain diary and putative “neuropathic pain questionnaires” if time is limited. There are mobile apps to track pain levels and daily events, assuming the patient fills them out properly.
Like what you’re learning? Take it a step further and test your clinical diagnosis skills with USC’s Virtual Patient Simulation. Review real-life patient histories, symptoms, and imaging, conduct a medical interview and clinical exam, make a diagnosis, and create a treatment plan for virtual patients experiencing Orofacial Pain conditions.

Dental Neuropathic Pain (NPP) Questionnaire
There are several suggested neuropathic pain questionnaires in the literature, but so far no one has created one exclusively for trigeminal neuropathic pain. This process was started in 2013, by Durham and colleagues, but it has not yet resulted in a validated NPP questionnaire for Persistent Dento-Alveolar Pain (PDAP). Examine the S-LANSS questions below if you want to incorporate NPP type questions into your clinical interview rather than use a self-report questionnaire.
Persistent Dento-Alveolar Pain Study
In this study, 20 cases of Persistent Dento-Alveolar Pain (PDAP) were identified from a database, DurhamJ, et al. conducted semi-structured interviews with the patients, recorded the interviews, and transcribed them verbatim.
Results
Several themes emerged including difficulty in responding to history taking, duration and magnitude of pain, complex and confounding descriptors, and common exacerbating factors.
Limitations of Neuropathic Pain Questionnaires
Mathieson S, et al. reviewed 37 studies on neuropathic pain screen questionnaires to test their measurement properties and found that the French DN4 assessment and English NPQ assessment tools had good overall qualities. They found the ID Pain assessment had good reliability, but was otherwise poor. They found the LANSS to be unsatisfactory, and PainDETECT had good Ho testing and validity.
Mathieson S, et al.’s conclusion was the DN4 Questionnaire and NPQ were most suitable for clinical use, although these screening questionnaires can not replace a thorough clinical assessment.
Differentiating Nociceptive Pain and Neuropathic Pain
While there is no Neuropathic Pain questionnaire that is specific for orofacial pain, in 2001 a questionnaire was developed that partially differentiates nociceptive pain from neuropathic pain.
Self-Reported Leeds Assessment of Neuropathic Symptoms and Signs (S-LANSS) and NPS Scale Questionnaire
In this study, 200 patients with chronic pain were asked to complete the S-LANSS questionnaire unaided. The S-LANSS assessment is a self-reported version of the questionnaire while the NPS assessment tool is an interview format version.
Then, an independent clinician determined the pain type (neuropathic or nociceptive), and then the certainty of the diagnosis was rated by the independent clinician. The S-LANSS questionnaire was also added to a chronic pain questionnaire that was sent to 160 community patients and 150 newly referred patients waiting for a pain clinic assessment.
This study found that the S-LANSS scale correctly identified 75% of pain types when self-completed, and 80% of pain types using the NPS format for the S-LANSS questionnaire.
The study found:
- The sensitivity for self-completed S-LANSS scores ranged from 74% to 78%.
- The NPS score and the S-LANSS scores were highly correlated.
- In the postal survey, completed questionnaires were returned by 57% of patients (n = 174).
- Internal consistency and convergent validity of the survey S-LANSS scores were confirmed.
These findings support the S-LANSS scale as a valid and reliable self-report instrument for identifying neuropathic pain and it is also acceptable for use in postal survey research.
Continue your Education Online: Dental Graduate Programs
Do you want to deliver appropriate and safe care to your growing and aging dental patients? Consider enrolling in USC’s competency-based Master of Orofacial Pain and Oral Medicine degree program to earn while learn.
