Systemic Diseases
Many systemic diseases are reported to cause or be associated with salivary gland hypofunction as mentioned in Table 1 [29], [64].
Of these systemic diseases, Sjogren’s syndrome (SS) is the most common disease that causes both xerostomia and salivary gland hypofunction with the incidence of xerostomia in the SS patient reaching nearly 100% [29], [65].

SS is a chronic, autoimmune disease that is characterized by progressive injury to the exocrine glands, mainly the lacrimal glands and the salivary glands. Although the exact mechanism of SS is not known, it is associated with B lymphocyte hyper-reactivity, autoantibody production and T-cell lymphocytic infiltration to exocrine glands and other organs [65].
SS may present as a primary disease or a secondary disease that is associated with other autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis [64], [65].
All ages can be affected by SS but it generally becomes overt during the fourth and fifth decade of life [65] and elderly patients account for up to 20% of Sjogren’s cases [29].
As the HIV infected population ages, more salivary conditions are being noted as a result of the HIV virus or the anti-retrovirals used for its treatment. Mulligan et al. also found that women who are HIV positive presented salivary gland disease manifested by glandular enlargement, tenderness, and absence of saliva on palpation [66].
Table 1: Etiology or Causes of Salivary Gland Hypofunction and Xerostomia [25], [29], [44], [46], [58], [64], [65].
| Preparation | Products | Active Ingredients |
|---|---|---|
| Sugarless Chewing Gums | Biotene dry mouth gum (GlaxoSmithKline) Orbit (Wm. Wrigley Jr. Company) Eclipse (Wm. Wrigley Jr. Company) Extra (Wm. Wrigley Jr. Company) Trident/Stimorol (Mondelēz International) Ice Breakers (The Hershey Company) Xylifresh (Leaf International) Spry Xylitol Gum (Spry Dental Defense System) Smint (Perfetti Van Melle) Salix SST (Scandinavian Natural Health & Beauty Products, Inc) | Sorbitol, Xylitol, Maltitol Sorbitol, Mannitol, Xylitol Maltitol, Sorbitol, Mannitol Sorbitol, Mannitol, Maltitol Xylitol, Sorbitol, Mannitol Xylitol Xylitol Xylitol, Sorbitol Xylitol Sorbitol, fruit acid |
| Sugarless tablets/discs/patches | Xylimelts (Orahealth Corporation) | Xylitol |
| Sugarless solution/spray | Mouth-Kote (Parnell Pharmaceuticals, Inc.) | Yerba santa, Xylitol, lemon oil |
| Sugarless hard candy, mints, lozenges or lemon drops | Many preparations available - Trident, Spry, Smint, ACT, etc. | Sugar substitutes, citric acid, etc. |
Radiation Therapy Effects
Another major cause of dry mouth is head and neck radiation with or without chemotherapy for cancer treatment near salivary glands.
Radiotherapy in the head and/or neck region can cause temporary or permanent damage to the salivary glands [25], [29], [58], [65], [67]. Salivary flow rates were the most severely reduced in patients with a history of radiation therapy when compared with patients with SS patients or patients on xerogenic medications [68].
Once head and neck radiation therapy is begun, salivary gland flow decreases as does oral health related quality of life; these reductions often continue on a chronic basis and may result in a lifelong condition [68], [69].
The prevalence and the severity of xerostomia and salivary gland hypofunction in head and neck cancer patients depends on the tumor site, stage, type of radiation therapy, the cumulative dose of irradiation, and the volume of salivary gland tissue included in the treatment portals [69].
The highest prevalence and severity of salivary gland hypofunction and xerostomia has been reported in nasopharyngeal [29], [69] and oropharyngeal carcinoma where all salivary glands bilaterally are included in the radiation treatment.
In contrast, the least prevalence of these conditions are when the cancer is located in the laryngeal/epilaryngeal area, which is more remote from the salivary glands [69].
Conventional radiotherapy doses of ∼60 Gy to the glandular tissue results in high rates of tissue destruction and the described sequelae [69]. The treatment of head and neck cancer with radiation usually is extended over 5–7 weeks and includes a total dose of 50–70 Gy delivered in daily allotments of 1.8–2.0 Gy [70].
Salivary flow begins to be impacted fairly quickly after initiation of therapy, falling to 50–70% of baseline once 10–16 Gy is delivered. Flow becomes nearly undetectable after the cumulative doses of 40–42 Gy [68], [70].
Radiation induced salivary hypofunction is accompanied by changes in the composition of saliva, including the lowering of salivary pH and therefore buffering capacity; and decreases in amylase activity, while at the same time it demonstrates increasing osmolality and viscosity, and higher concentrations of lactoferrin, protein, sodium, chloride, alterations in mucin and calcium concentration [29], [70].
Using 3D conformal radiation therapy can reduce the radiation dosage to the contralateral parotid gland and Intensity-Modulated Radiation Therapy (IMRT) allows more accurate delivery of specific radiation dosage and distribution to the tumor mass, while sparing the salivary glands. By doing so, both 3D conformal radiation therapy and IMRT can decrease the prevalence and severity of radiation induced salivary hypofunction [69].
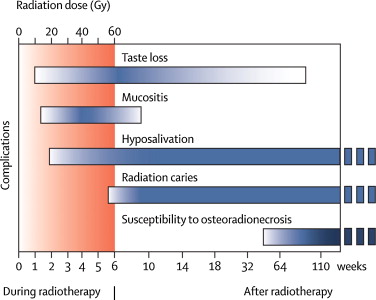
In addition to salivary hypofunction, there are other head and neck radiation induced outcomes that can occur including taste loss, mucositis, radiation caries and susceptibility to osteonecrosis of the jaw bone, all of which can negatively impact oral health related quality of life (Fig. 1) [64], [69], [71].
Other treatments for cancer such as radioactive iodine therapy, total body irradiation/chemotherapy and hematopoietic stem cell transplantation, chemotherapy, and immunotherapy have also been reported to have the potential of causing dry mouth but there is not sufficient data to report on the severity and grading of the resulting dry mouth outcomes [69].
Postgraduate Degrees in Geriatric Dentistry
Are you looking for improved ways to diagnose, treat, and manage the oral healthcare of older patients? Explore the Herman Ostrow School of Dentistry of USC’s online master’s and certificate program in Geriatric Dentistry.
About the Authors
The article, “Dry mouth: A critical topic for older adult patients,” was authored by Phuu Han, Piedad Suarez-Durall, and Roseann Mulligan, Director Geriatric Dentistry Master and Certificate programs at the Herman Ostrow School of Dentistry of USC, and was originally published by Elsevier in the Journal of Prosthodontic Research.
References
[25] C. Scully
Drug effects on salivary glands: dry mouth
Oral Dis, 9 (2003), pp. 165-176
[29] B. Liu, M.R. Dion, M.M. Jurasic, G. Gibson, J.A. Jones
Xerostomia and salivary hypofunction in vulnerable elders: prevalence and etiology
Oral Surg Oral Med Oral Pathol Oral Radiol, 114 (2012), pp. 52-60
[58] S.R. Porter, C. Scully, A.M. Hegarty
An update of the etiology and management of xerostomia
Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 97 (2004), pp. 28-46
[64] P. Tschoppe, M. Wolgin, N. Pischon, A.M. Kielbassa
Etiologic factors of hyposalivation and consequences for oral health
Quintessence Int, 41 (2010), pp. 321-333
[65] Y. Peri, N. Agmon-Levin, E. Theodor, Y. Shoenfeld
Sjögren's syndrome, the old and the new
Best Pract Res Clin Rheumatol, 26 (2012), pp. 105-117
[66] R. Mulligan, M. Navazesh, E. Komaroff, D. Greenspan, M. Redford, M. Alves, et al.
Salivary gland disease in human immunodeficiency virus-positive women from the WIHS study. Women's Interagency HIV Study
Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 89 (2000), pp. 702-709
[67] J. Kałużny, M. Wierzbicka, H. Nogala, P. Milecki, T. Kopeć
Radiotherapy induced xerostomia: mechanisms, diagnostics, prevention and treatment – evidence based up to 2013
Otolaryngol Pol, 68 (2014), pp. 1-14
[68] M.A. Cho, J.Y. Ko, Y.K. Kim, H.S. Kho
Salivary flow rate and clinical characteristics of patients with xerostomia according to its aetiology
J Oral Rehabil, 37 (2010), pp. 185-193
[69] S.B. Jensen, A.M. Pedersen, A. Vissink, E. Andersen, C.G. Brown, A.N. Davies, et al.
A systematic review of salivary gland hypofunction and xerostomia induced by cancer therapies: prevalence, severity and impact on quality of life
Support Care Cancer, 18 (2010), pp. 1039-1060
[70] T.L. Lovelace, N.F. Fox, A.J. Sood, S.A. Nguyen, T.A. Day
Management of radiotherapy-induced salivary hypofunction and consequent xerostomia in patients with oral or head and neck cancer: meta-analysis and literature review
Oral Surg Oral Med Oral Pathol Oral Radiol, 117 (2014), pp. 595-607
[71] A.M. Kielbassa, W. Hinkelbein, E. Hellwig, H. Meyer-Lückel
Radiation-related damage to dentition
Lancet Oncol, 7 (2006), pp. 326-335
