Learn how to conduct a comprehensive dental exam of a new patient who might be suffering from Obstructive Sleep Apnea.
Comprehensive Dental Exam for New OSA Patients
Below are the elements of a physical examination that should be conducted when assessing a possible OSA patient.
1. Measurement of Jaw Opening
Set a millimeter ruler against the lower teeth, and instruct the patient to “even if it hurts, open as wide as you can.” Measure from the top of the lower incisors to the incisal edge of the upper incisors.
If the opening is less than 40 mm also add in overbite distance to the final measurement. When a patient has limitation (<40mm) then find out if the limitation is recent and what is the likely source of the limitation.
Like what you’re learning? Take it a step further and test your clinical diagnosis skills with USC’s Virtual Patient Simulation. Review real-life patient histories, symptoms, and imaging, conduct a medical interview and clinical exam, make a diagnosis, and create a treatment plan for virtual patients experiencing Orofacial Pain conditions.

2. Lateral and Protrusion Motion of the Jaw
Instruct the patient to “without opening wide, move your jaw as far as you can to the right (or left).” Use a millimeter ruler to measure the distance between the midlines. If the midlines are not coincident with the teeth in full intercuspation, select the appropriate point on the mandible that corresponds to the maxillary midline and measures this distance when the jaw is shifted to the side.
When a patient has a limitation (<8mm) laterally then find out if the limitation is recent and what is the source of the limitation.
3. Auscultation of TM Joints for Sounds:
Use a stethoscope to determine if a patient has temporomandibular joint noises. The patient should open and close their mandible. If a TMJ click is produced, it should be palpable. If the noises are crepitation like sounds record this. Never record as positive any sound the patient cannot verify as being present since false positives are not uncommon.
Occasionally it may be necessary to load the joint to induce some of the sounds which patients report as being only sometimes present with eating. Sound detected are recorded as a single motion click, a multiple clicks or a grinding noise (crepitation).
Like what you’re learning? Download a brochure for our Orofacial Pain and Oral Medicine certificate or master’s degree program.
4. Masticatory Muscle Tenderness
Muscle palpation is done bilaterally using steady firm pressure (2 kg of pressure) for 1-2 seconds. Ask the patient to rate the tenderness (if any) that is produced with this pressure using a 0 for none; 1 for mild; 2 for moderate; and 3 for severe tenderness.
When you palpitate the muscle check for tenderness and examine iy to see if it has a taut band which runs parallel to the direction of the muscle fibers. To do this examination, it is presumed the examiner knows the landmarks need to identify the underlying muscle.
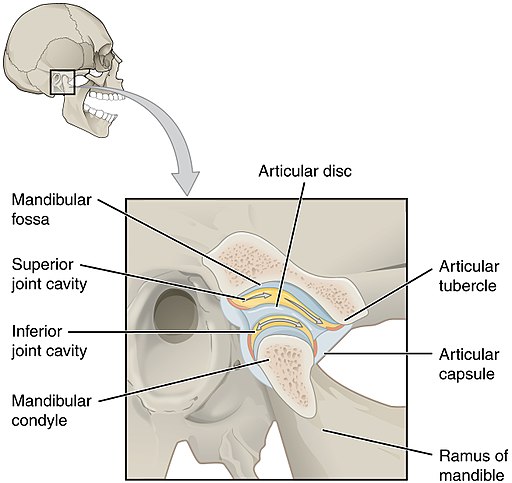
5. Temporomandibular Joint Palpation for Tenderness
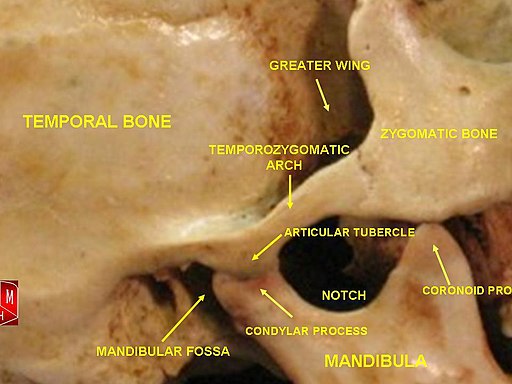
The examiner must first place their index finger just in front of the tragus of the ear, ask the patient to open slightly feeling for the lateral pole of the condyle. The examiner applies 1kg (2.2 lbs) of pressure to the joint asking the patient to rate if this pressure causes no pain, mild, moderate, or severe pain.
The dorsal aspect of the condyle and is tested by asking the patient to open wide or fully protrude the jaw. This allows the examiner to feel around behind the condyle and thus palpate its dorsal aspect.
Dorsal palpation of the condyle can also be performed with the patient’s mouth closed. Insert your smallest finger into the external auditory meatus, and forward pressure is applied to the back of the condyle, making sure not to compress the tragus cartilage.
6. Occlusal Examination – Attrition
Now examine the anterior teeth for substantial attrition by first drying the teeth with air and or cotton & inspect them carefully with under direct or reflected light with a mouth mirror. Extend your attrition examination to the posterior teeth again drying them and using a mouth mirror inspect them for polished facets.
Usually, teeth are rated as having:
- 0 = no wear;
- 1 = enamel wear only;
- 2 = enamel wear with dentin exposure but less than 1/3 of clinical crown lost;
- 4 = more than 1/3 of clinical crown loss.
Sometimes you see erosion on the anterior and posterior teeth that can be mistaken for attrition, but erosion involves cupping of exposed dentin and this can not be done by attrition.
7. Mucosal Tissue Exam

First, the examiner inspects the inner surface of the lower lip and the anterior gingival attached tissues and vestibule of the lower anterior labial region. Move to inspect the right/left buccal mucosa to include the parotid duct. This is done by pulling the buccal mucosa away from the teeth with the fingers and visualize this tissue under direct light.
After this, the examiner inspects the attached maxillary and mandibular buccal gingival tissues and vestibules on the right and left sides. Moving forward again, the examiner lifts up the upper lip and inspects the maxillary lip mucosa and labial attached gingival and vestibule. After this, the examiner inspects the entire hard and soft palate.
8. Occlusal Stability
To certify that the patient has a normal occlusion, several examination procedures must be completed. The examiner begins by checking for dental midline symmetry by identifying the maxillary and mandibular midlines and seeing how they line up with the teeth in full intercuspation or ICP. It is necessary to cross-check the maxillary midline with the facial midline to see that they are similar before deciding if the mandibular midline is off-center.
9. Periodontal/Caries Exam for Local Disease
Dental appliance for sleep apnea should not be considered if the patient has untreated substantial periodontal or dental disease. Inspection of the teeth for broken fillings, inadequate restorations, caries, or periodontal disease is necessary.
10. Nasal Airway Obstruction
This examination is more functional than visual. The patient is asked to block one nostril and then inhale deeply through the open nostril. Inability to demonstrate nasal patency would suggest an ENT consult might be required.
11. Palate/Uvula Length and Inflammation

After depressing the tongue with a tongue depressor, ask the patient to say “ah.” This will elevate the soft palate. The problematic patient is the one where it is impossible to visualize the end of the soft palate or uvula. Some patient will demonstrate a highly inflamed (erythematous) uvula and soft palate or possibly enlarged tonsils.
12. Substantially Enlarged Tonsils
When the tonsils are large enough that they may restriction airflow, the patient will require an ENT consult.
13. Substantial Micrognathia
Sagittal view of the patient will help determine if the patient has a shortened lower jaw (micrognathia). These cases might require a referral to an oral-maxillofacial surgeon.
14. Excessively Large Tongue
There is no standard tongue measuring measurement method, but large tongues are like good art, you know it when you see it. There is generally nothing that can be done about a large tongue short of surgical resection, but when you see one, the prognosis that the dental appliance will be highly effective is lower.
Earn an Online Postgraduate Degree in Orofacial Pain and Oral Medicine
Are you interested in a variety of issues focused on orofacial pain, medicine and sleep disorders? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Orofacial Pain and Oral Medicine.

