Today we’re talking about COVID-19’s impact on nursing home residents that goes beyond what you might have heard in the news. Please find the recorded lecture, the PowerPoint presentation, and a formatted transcription of the lecture below.
Don’t have time to read the full article? Download the Healthcare Provider’s Guide to Caring for Vulnerable Populations During COVID-19.
What Types of Care do Nursing Homes Provide?
People go to nursing homes for a variety of reasons, and the services that they provide, I would categorize into two different aspects. One is the physical, and one is the psychological, in order to ensure the well-being of the residents.
Physical Care
For example, there’s care, vigilance, and protection. That’s one of the physical attributes provided by the nursing home, as well as around-the-clock healthcare, therapy, medication distribution, assessment, and a whole variety of medical services. Additionally, there are so many instrumental activities of daily living that are provided as part of taking care of the physical part of the resident.
Psychological Care
Nursing homes provide psychological care as well. But it’s not just care in therapy and psychological therapy, but the psychological care extends through a variety of activities that are provided. For example, group activities: it could be art, games, exercise, etc. It can be a variety of things that help improve the patient’s psychological well-being.
Eating meals communally helps contribute to socialization. It provides an opportunity for residents to meet other people in their cohort and to make new friends and relationships. It gives them a place to visit with their friends, their family, and, in general, provide sensory stimulation. All those things are part of the psychological support that nursing homes provide.
Like what you’re learning? Download a brochure for our Geriatric Dentistry Master Program certificate or master’s degree program.
COVID-19’s Impact on Nursing Home Residents
What’s happening now with COVID-19 in nursing homes is a lot of this has changed, and this isn’t just a United States phenomenon, but something we’re seeing around the world where there are nursing homes and vulnerable populations.
The impact for COVID-19 has decreased meaningful socialization for the residents and in the activities of their existence. Therefore, it’s decreased the stimulation. The downside of that is it has increased mental health issues. Things like depression and anxiety are much, much greater now in our nursing home residents than they were before the epidemic. We even see a worsening of the dementia for a variety of reasons.
Ultimately, the end result is a failure to thrive of the resident that could result in their giving up – or be a contributing factor to their giving up – and seeing an indirect death rate as a result of COVID-19 versus the direct death rate that you hear about on the news from the virus directly infecting various systems in their body.
Social Isolation vs. Loneliness
Let’s just define a little bit the difference between social isolation and loneliness.
Social isolation is the objective finding of a lack of social contact with others, whereas loneliness is that perception of social isolation or the subjective feel of being lonely. What does lonely mean? Lonely means without companions; a solitary existence.
Are Social Isolation Loneliness the Same?
No, they’re not. But they have a lot of overlap. For example, not 100% of people who are socially isolated are depressed, but there is 50% who are. There is overlap, but not total overlap. But when you have depression, for example, we know that suicide rates go up. We also know that depression and loneliness contribute to increases in dementia.
Social isolation and loneliness is also interestingly associated with elevations of physical findings including elevated cardiovascular risk and neuroendocrine markers of stress. This whole time, we think it’s stressful for us? It’s stressful for nursing home residents as well.
Disrupted sleep is another finding that we see associated with social isolation and loneliness. Then the pro-inflammatory physiologic markers affecting acceleration of neurodegenerative changes are some of the additional things that we find.
Nursing Home Activities: How Can We Improve Quality of Life?

1. More family phone calls.
Right now, the caregivers, the aides, are impacted, but we need them to help manage the mechanical and the logistical contact of the families for these phone calls, and more frequent phone calls. Same with video chats. We typically need the aides to help out there. But we need them in other areas, too. We need them to help with maintaining the social isolation, social distancing when families come. That’s important as well.
2. Therapeutic Animals
Do therapeutic animals through the windows help? We don’t know, but we know we can’t bring therapeutic animals in anymore because we know that they can contract COVID-19 and bring it into the facilities. Seeing them through windows, is that adequate? Don’t know.
3. Voice Recordings of Family Members
Voice recordings of family members that the resident could hear over and over might be one solution. Asking the family to bring in and leave photo albums so that the resident can enjoy those memories and maybe talk about them to other residents would be another idea.
4. Closed-Circuit Broadcasting to Each Room
I’m aware of a nursing home facility that took some of their residents who are more able and have them act as disc jockeys to play music from the time era that their residents would know for an hour every day. That can be piped into the resident’s room for a change of pace.
Challenges
Many of these things that have been suggested are great ideas, but we have some obstacles to institute in them.
Social Distancing Compliance
First of all, again, we’ve got to keep the social distancing and any new protocols in place, whatever is dreamed up for an activity. Remember, too, that the staff have to be screened every day, which is going to take away some staff time from their ability to do things with the residents. Everybody has to be regularly tested for COVID-19, whether it’s staff, residents, or ultimately any visitors that are allowed in. More staff are needed, not fewer.
In some of the nursing homes that have been very hard hit with many staff being out ill, others have to be brought in. For example, when the governor of our state brought in the military reserves to help in nursing homes with just basic needs.
Personal Protective Equipment (PPE)
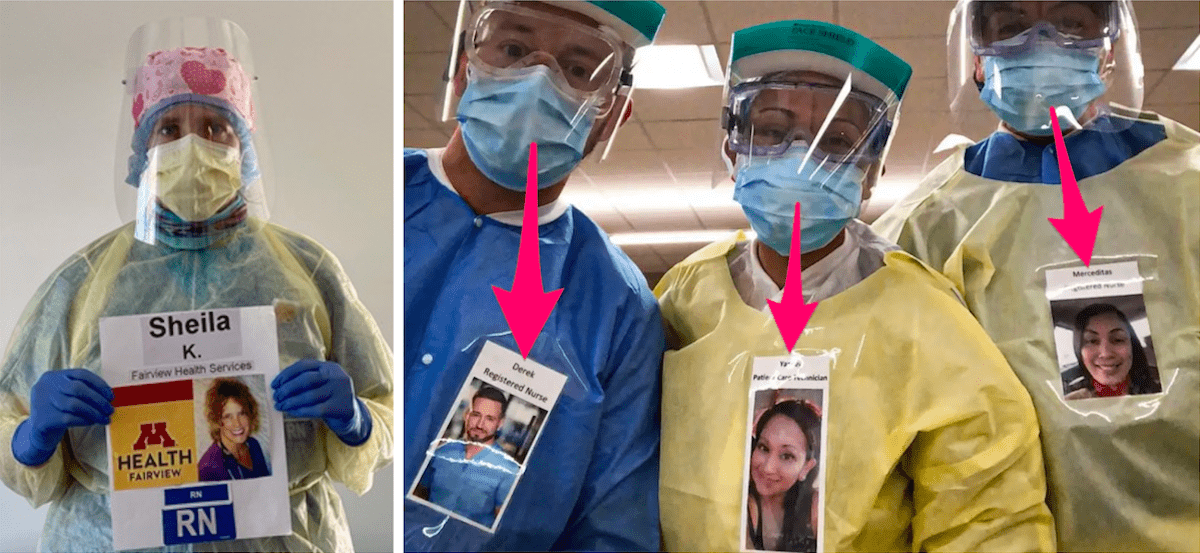
Remember, too, that there has been an issue of not having enough PPE, and that’s to protect the staff, but also PPE is stressful for the patients because frequently patients don’t understand what’s going on. “Why are you wearing all this gear?” They can’t see social cues, smiling, and they can’t always hear what’s being said and muffled by the mask. It’s stressful and impedes communication.
As a result, new and disruptive behaviors can pop up that result in psychotropic medications being given, which is not the best for our nursing home residents. When there are new cases in the facilities, the facilities have to react by isolating even further, which leads to further isolation and potentially depression.
Related Reading: Pain Researchers Help Understand COVID-19 Treatment
Engaging the Demented Patient
1. Window Visits
Window visits seemed like a good idea, and one of the first things as a solution that came up. But window visits may not be here helping, particularly for the demented patient because they don’t understand what’s going on. Why can’t they touch? Why can’t they be touched? Why can’t they hug? Why can’t they kiss and be kissed? It can be very confusing.
That’s what has been discovered from this great idea that didn’t always work. Being unable to understand. If you have the families coming and the residents wearing masks, but they don’t understand why they’re wearing a mask and it’s annoying, and so they just take it off. That’s another area that has been problematic, and just staying that six feet apart.
Related Reading: How to Support Geriatric Patients with Dementia and COVID-19
2. Go Outside
One alternative that has been more recently shown to be beneficial is to go outside. Don’t do things inside where the virus can be more readily transmitted if it happens to be there. For example, occupational therapy and physical therapy sessions can be held outside.
3. Live Music
What about having live music outside? Many musicians don’t have gigs and they’re playing on their porches, in their homes, or for the neighbors. Maybe some of them would like an audience and want to play outside to nursing home residents.
Alternative Options
Anything to add variety and interest to the day are good alternative options for supporting the nursing home residents.
- Parades
- Taking meals outside
- Outdoor walks one-on-one with an aide
- Outdoor family visits
Engaging the Community
A nursing home in Culver City, Marycrest Manor, ingeniously came up with a safe 4th of July event for their residents. Because fire engines have to be taken out every now and then, Marycrest Manor invited their local fire department to come and do a drive-by.
They had all of the residents up on the deck where they could see the fire truck, and they all drove by – the hook and ladder, the EMT vehicle, the chief’s car, etc. Everybody had their flags, because it was near 4th of July, they had signs out saying, “Thank you, first responders,” and the fire folks beeped their sirens a little bit. It gave a very exciting time and made a difference to a day in the life of a nursing home resident.
That’s an update on what’s happening with our nursing home residents that goes beyond what you see in the headlines, all the deaths in the paper, and how much socialization plays an extreme role in keeping our nursing home residents healthy, happy, and having a good quality of life. That’s what they’re missing right now.
Postgraduate Geriatric Dentistry
Are you looking for improved ways to diagnose, treat, and manage the oral healthcare of older patients? Explore our online master’s and certificate program in Geriatric Dentistry.



