Tooth extraction remains one of the most common dental procedures, yet it carries increased risks for patients with chronic systemic conditions such as diabetes and cardiovascular disease. Approximately one in ten patients experience adverse events in healthcare settings. The risk of these events is often higher in patients with moderate systemic conditions, as their medical complexity requires oral health providers to communicate explicitly in ways that support patient understanding [1]
Patients classified as ASA II and III, commonly those with chronic conditions like cardiovascular disease or diabetes, are at higher risk for delayed wound healing, infection, and bleeding complications after dental procedures. As the global prevalence of disease continues to rise, dental professionals should consider what is the best effective patient-centered communication in perioperative care with their patients [2].
Effective patient communication evolves into patient education, which supports best practices for reducing postoperative complications. Clinical protocols must give significant attention to selecting communication specifically for patients with chronic conditions. This blog offers a brief overview of how oral health providers can use behavioral and learning theories to improve patient communication with ASA II and ASA III patients, aiming for best post-operative outcomes [3].
Like what you’re learning? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Community Oral Health.
Communicating Post-Extraction Instructions
Systemic conditions, such as diabetes and cardiovascular disease, can significantly impact healing after tooth extractions, making clear, patient-centered communication essential. For example, patients with diabetes may not realize that poor blood sugar control can delay healing or increase the risk of dry socket. Similarly, those with cardiovascular disease, especially individuals on anticoagulants or with a history of heart conditions, face heightened risks if postoperative instructions are misunderstood or not followed. Clinicians must translate complex medical considerations into plain, actionable language, emphasizing the ‘why’ behind each instruction [4]. Instead of listing precautions, explain that taking medications as directed, managing blood pressure, and avoiding certain activities support the body’s ability to form a healthy blood clot, which is imperative for healing. For patients with chronic conditions, it is recommended to use visual aids, written summaries, or follow-up reminders for effective communication. With ASA II and III, poor comprehension or adherence is a safety risk that can lead to avoidable complications and emergency care.
The Role of Communication in Postoperative Care
Effective communication of postoperative care is a collective responsibility that involves the entire dental team; however, clinicians bear the primary duty to initiate, guide, and structure patient education. Provider behaviors such as tone, language, setting, and pacing directly influence patient understanding and recall. Effective communication must translate into correct post-operative care for chronic disease patients whose healing depends on strict adherence. Patients often struggle to recall detailed instructions when they are anxious or overwhelmed [5]. Clinicians must deliver information clearly and in manageable segments tailored to individual patient needs and ensure, to the best of their ability, that the patient is following the dialogue. When communication is delivered using a theoretical foundation a personalized approach can be increase the likelihood of patient compliance.
Applying the Health Belief Model to Achieve Best Outcomes
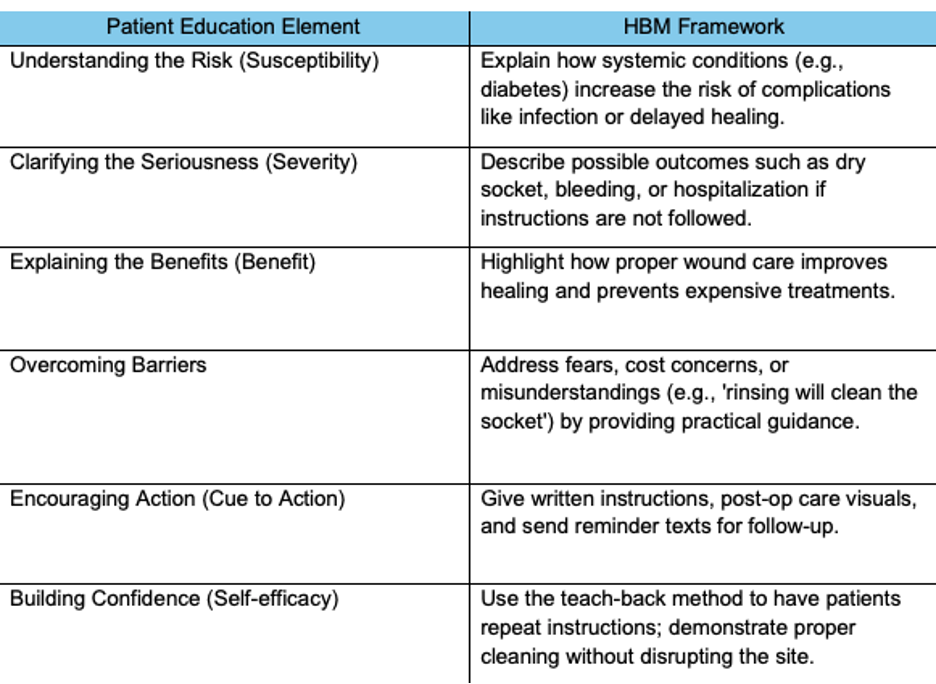
The Health Belief Model (HBM) offers a framework for understanding patient decision-making and motivating adherence [6]. The model proposes that individuals are more likely to engage in health-promoting behaviors when they:
- Recognize their vulnerability to a health threat (susceptibility)
- Understand the seriousness of potential consequences (severity)
- Believe that specific actions will yield benefits
- Identify and overcome barriers to action
- Receive prompts that encourage behavior (cues to action)
- Build confidence in their ability to perform recommended actions (self-efficacy)
In postoperative care for ASA II and ASA III patients, the model helps clinicians connect systemic conditions with the risks and benefits of healing. For example, explaining to a diabetic patient how uncontrolled blood sugar delays healing and increases infection risk makes instructions relevant and urgent.
Given that approximately 10% of patients experience adverse events in healthcare, applying a structured framework like the Health Belief Model (HBM) can help oral health providers improve postoperative communication. The HBM offers a guide for developing effective communication strategies by recognizing how patients’ beliefs shaped by their understanding of health information influence their perception of risk, motivation to follow instructions, and likelihood of adhering to postoperative care, promoting safer outcomes.
Figure 1.
Using the Health Belief Model to Guide Patient Communication and Support Healing After Tooth Extraction
Constructivist Learning: Actively Engaging the Patient
Constructivist Learning theory enhances postoperative communication by encouraging active patient involvement. Patients learn and understand best when new information connects to their experiences and behaviors. Oral health providers initiate patient comprehension by asking reflective questions about daily routines, such as glucose monitoring or blood pressure management, and how these affect healing. [7].
Encouraging patients to express understanding or concerns builds trust and allows clinicians to correct misunderstandings before complications occur. A patient-centered approach values and respects diverse backgrounds and varying comprehension levels, which is significant for medically complex populations. Clinicians can create effective communication using teach-back methods, where patients explain instructions in their own words, reinforce understanding, and increase confidence [8].
Five Practical Evidence-Based Communication Tips for Clinicians
- Teach-Back Method: Confirm comprehension by asking patients to repeat instructions in their own words. This feedback loop allows clarification and reinforces key points.
- Visual Infographics: Use charts or diagrams illustrating healing timelines for controlled versus uncontrolled systemic conditions. Visual aids help patients conceptualize the importance of adherence.
- Step-by-Step Care Sheets: Provide patients with a checklist of daily postoperative tasks to follow. Structured formats reduce cognitive overload and serve as reliable reference points for at-home use [5].
- Relatable Metaphor: Help patients understand complex ideas [9].Suggestion: explain a blood clot metaphorically… It’s like your body’s invisible bandage.
Additionally, follow-up messages may bescheduled phone calls or texts 24 hours after extraction. Proactive outreach can address forgetfulness, language barriers, and stress that often obstruct effective postoperative care [5].
Communication Is Clinical Care
Effective communication extends to the entire oral health dental care team, including dentists, hygienists, assistants, and administrative teams. Consistent messaging, structured tools such as checklists, and shared protocols enhance continuity and reduce confusion [5]. Studies reveal that communication failures and poor team coordination contribute more to adverse outcomes than just technical errors. Implementing clear communication frameworks based on behavioral and learning theories can reduce preventable harm and support equitable care for medically complex patients.
The Health Belief Model guides discussions of risks and benefits, and the application of constructivist learning to encourage personal reflection and helps make postoperative instructions effective [10].
Suggestion for oral health providers:
- Use the Health Belief Model to create communication and education for patients to relate postoperative care instructions to their personal perceptions and beliefs, reinforcing the desired health behavior, in this case, adherence to postoperative instructions
This blog is an adaptation of a final course assignment created by Dr. Farzaneh Delpisheh Mobashery in the Master of Community Oral Health Program, Spring 2025 semester.
Earn an Online Postgraduate Degree in Community Oral Health
Do you like learning about a variety of issues while focused on the unique needs of community health dental programs? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Community Oral Health.
References
[1] J. Howick, A. Bennett-Weston, J. Solomon, K. Nockels, J. Bostock, and L. Keshtkar, “How does communication affect patient safety? Protocol for a systematic review and logic model,” BMJ Open, vol. 14, no. 5, Art. no. e085312, 2024, doi: 10.1136/bmjopen-2024-085312.
[2] K. Gupta et al., “Dental Management Considerations for Patients with Cardiovascular Disease—A Narrative Review,” Reviews in Cardiovascular Medicine, vol. 23, no. 8, Art. no. 261, 2022, doi: 10.31083/j.rcm2308261.
[3] J. W. Little, D. Falace, C. Miller, and N. L. Rhodus, Dental Management of the Medically Compromised Patient, 10th ed. St. Louis, MO: Elsevier, 2012.
[4] T. O. Aremu, O. E. Oluwole, K. O. Adeyinka, and J. C. Schommer, “Medication Adherence and Compliance: Recipe for Improving Patient Outcomes,” Pharmacy, vol. 10, no. 5, p. 106, 2022. doi: 10.3390/pharmacy10050106
https://doi.org/10.4159/9780674419377
[5] V. Sameera, A. Bindra, and G. Rath, “Human errors and their prevention in healthcare,” Journal of Anaesthesiology, Clinical Pharmacology, vol. 37, no. 3, pp. 328–335, 2021, doi: 10.4103/joacp.JOACP_364_19.
[6] B. S. Kam and S. Y. Lee, “Integrating the health belief model into health education programs in a clinical setting,” World Journal of Clinical Cases, vol. 12, no. 33, pp. 6660–6663, 2024, doi: 10.12998/wjcc.v12.i33.6660.
[7] M. Wijnen-Meijer, T. Brandhuber, A. Schneider, and P. O. Berberat, “Implementing Kolb’s Experiential Learning Cycle by Linking Real Experience, Case-Based Discussion and Simulation,” Journal of Medical Education and Curricular Development, vol. 9, pp. 1–7, 2022. https://doi.org/10.1177/23821205221091511
[8] L. Marks, L. O’Sullivan, K. Pytel, and J. A. Parkosewich, “Using a teach-back intervention significantly improves knowledge, perceptions, and satisfaction of patients with nurses’ discharge medication education,” Worldviews on Evidence-Based Nursing, vol. 19, no. 6, pp. 458–466, 2022. doi: 10.1111/wvn.12612
[9] P. C. Brown, M. A. McDaniel, and H. L. Roediger, Make it Stick: The Science of Successful Learning. Cambridge, MA: The Belknap Press of Harvard University, 2014.
[10] J. J. N. Tien, H. C. Tan, C. T. Chua, Y. M. Lee, and P. C. Tho, “Implementing an evidence-based structured education and management program in an inpatient adult oncology setting to improve patients’ pain control,” JBI Evidence Implementation, vol. 20, no. 4, pp. 326–333, 2022, doi: 10.1097/XEB.0000000000000309.


