This content was originally presented during the Herman Ostrow School of Dentistry of USC’s 2020 Geriatric Boot Camp. The original presentation can be found below, as well as an adapted write-up of what we covered in our session.
Don’t have time to read the full article? Download the Healthcare Provider’s Guide to Caring for Vulnerable Populations During COVID-19.
Impact of COVID-19 on Older Patients
The risk for severe illness from COVID-19 increases with age and older adults are at a higher risk. The CDC reports, 8 out of 10 COVID-19 deaths in the US have been adults 65 years and older. They are also more likely to have severe illness from COVID-19 which means that persons diagnosed with COVID-19 may require hospitalization, intensive care, or a ventilator to help them breathe. Everyone has the potential to contract COVID-19 but the older you get, the chances of hospitalization increases.
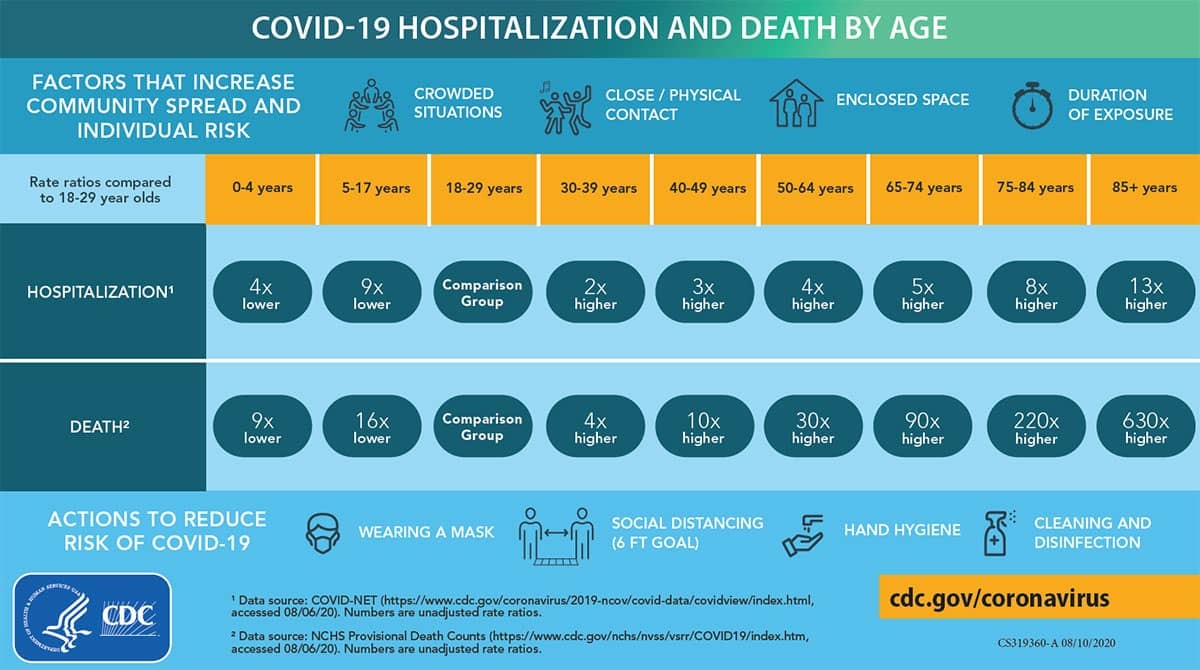
Source: CDC
People over 65 are five to thirteen times more likely to be hospitalized and 90 – 630 times more likely to die than 18-29-year-olds.
Impact of COVID-19 on Older Patients with Underlying Medical Conditions
Another group who are at a greater risk are those with underlying medical conditions – this one impacts any age group. Some of the medical conditions are cancer, chronic kidney disease, COPD, immunocompromised patients, obesity, sickle cell disease, type 2 diabetes, and serious heart conditions such as heart failure and coronary artery disease.
Supporting COVID-19 Patients with Dementia
While there is no evidence to cognitive deterioration due to COVID-19, there are psychological and behavioral changes. Today we’ll look at three different locations that a living with dementia would be in: the hospital, at home, and at an assisted living facility. We’ll explore what they might be experiencing and discuss some ways to accommodate them.
What is dementia?
Dementia is a decline in memory and other mental abilities. It is not a normal part of aging and affects older people more often. While 7% of adults 60 and older have dementia, nearly 30% of those 85 and older. The two most common causes of dementia are Alzheimer’s disease and vascular dementia.
People living with dementia may have difficulties with memory, language, and decision-making abilities, and possibly changes in their mood like increased irritability, depression and anxiety. Depending on the level of cognitive functionality, the person living with dementia may need extra care. So the caregiver’s role is very important as well as the care that’s provided.
1. Hospital and ICU Settings
Generally speaking, some of the patients staying in hospitals may feel isolated as they are by themselves and there might be some discomfort and delirium.
One of the biggest causes of the confusion and insecurity is the environmental stimulus from the hospital setting. With all the personal protective equipment (PPE) that healthcare providers are now required to wear – the N95 mask, face shields, and isolation gowns – it can be intimidating. All the noise and machines also add to the stimulus.
Some facilities have started putting laminated pictures of healthcare providers on their gown so it’s less intimidating, but for someone who has recently changed their environment to see people coming in like this, it can be a bit jarring.
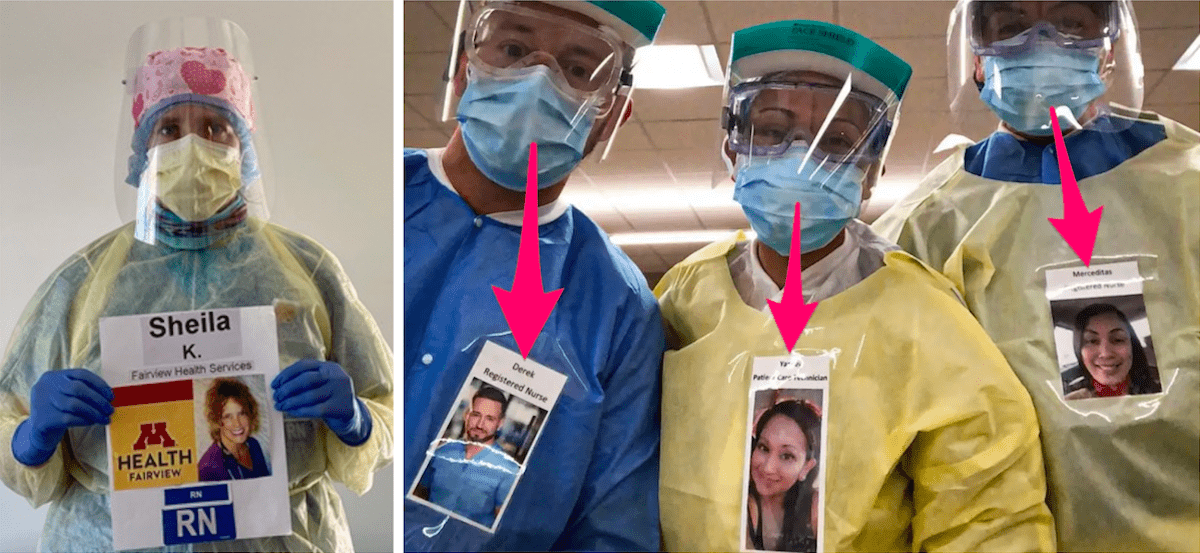
Imagine waking up and the first thing in the morning you see someone come into your room wearing all of this protective gear!
Environmental changes, isolated surroundings and somatic discomforts due to COVID-19 can cause sleep problems, increase anxiety, agitation and hostility. Patients may also exhibit episodes of delirium punctuated by acute changes in consciousness, impaired attention, sleep-wake cycle disturbances, abnormal sensory experiences, and emotional disturbances.
2. At Home
Many persons with dementia live at home and they cannot understand what is happening with the pandemic. Irrational analysis, changes with home care arrangements, disruptions in routine, and memory decline can add confusion, irritability, agitation, aggression, anxiety, stress, and tension to an already challenging care giving situation.
Unscheduled home life can lead to patients feeling bored due to limited activities and cause sleep disturbances that exacerbate existing challenges. A decline in memory and comprehension can lead to other issues like a poor understanding of infection control, a more disorganized daily life, an inability to cooperate with care, and even present conflicts with caregivers.
Like what you’re learning? Get more information about our online master’s and certificate program in Geriatric Dentistry.
3. Assisted Living Facilities
In assisted living facilities there is reduced face-to-face communication with family members, reduced interaction with caregivers, and a possibility that essential medications may be interrupted causing withdrawal symptoms.
For a lot of persons with dementia, increased confusion is usually the first symptom of any illness. If they show any rapid increased confusion, contact the healthcare provider first for advice. Unless the person is having difficulty breathing or high fever, it’s recommended to call the physician first instead of heading straight to the emergency room. There has also been noted some slower processing and a decline in usual abilities and function.
Some patients may demonstrate anxious and agitated behaviors or apathy, depression, and fatigue. Because hypoxia has been noted in COVID-19 patients, it may present with delirium. So there might be a change in consciousness, impaired attention, sleep/wake cycle disturbances, hallucinations, and other emotional disturbances.
Like what you’re learning? Download a brochure for our Geriatric Dentistry Master Program certificate or master’s degree program.
Impacts from Public Health Regulations

With COVID-19, some of the public health regulations have been put in place such as social distancing, emphasis on infection control, and stay at home orders. While these regulations are good for fighting the pandemic, they may have behavioral consequences.
Because a person with dementia might not fully comprehend what is going on, they might not be able to fully comply with all the changes, leading to them not being able to cooperate with hand washing or add to the confusion. Stay at home orders may also change daily life and routines causing increased day naps, sleep problems, and potentially wandering and pacing around the house.
On a positive note, with everyone staying at home, other family members may help with observations and watch after the person with dementia, which may lead to increased awareness of the individual’s limitations and challenges.
Questions to Help You Prepare
Here are some things to think about during the pandemic if the person with dementia gets sick:
- What provisions are available and in place?
- If they need to be quarantined at home, how will the caregiver minimize exposure?
- What additional conversations need to be had with friends, family, and neighbors to support the caregiver?
On the flip side, what if the caregiver gets sick?
- Who will care for the person with dementia?
- Where will the person with dementia be cared for?
- Is there a place to isolate the caregiver from the rest of the household?
- Who will handle medication management?
- How will the caregiver self-quarantine?
How can we help patients with dementia and families prepare?
Here are a few practical ways you can support persons with Dementia during the COVID-19 pandemic:
1. Establish a Routine
It would be helpful to establish a routine to minimize anxiety and behavioral issues. Some ways to accomplish this is to have regularly scheduled meal times and plan activities throughout the day like walking outside, reading, painting, cooking, or helping with laundry.
2. Reinforce Healthy Choices
It might be easy to park the person in front of the TV, nap all day and eat junk food, but this will just cause more problems. Try to limit the news and naps during the day and try to keep healthy snacks around.
3. Be Proactive
Try to anticipate behavioral changes, and be mindful that behavioral changes may indicate the person isn’t feeling well. If this happens, contact the doctor as soon as possible, especially if they have a fever, cough, or hard time breathing.
4. Put Up Written Reminders
To increase compliance with social distancing guidelines, put up written reminders around the house for frequent hand washing. If soap and water are not available, then at least 60% alcohol-based hand sanitizer should be used. Since social distancing may decrease the interaction they have with family members and friends, encourage phone calls and video calls to stay connected.
Postgraduate Geriatric Dentistry
Are you looking for improved ways to diagnose, treat, and manage the oral healthcare of older patients? Explore our online master’s and certificate program in Geriatric Dentistry.
References
- H. Wang. Dementia Care During the COVID-19 outbreak, Chinese J of Psychiatry 2020; 53
- A. Bianchetti. Clinical Presentation of COVID 19 in Dementia Patients, J Nutr Health Aging. 2020 May 15: 1-3
- Coronavirus (COVID-19): Tips for Dementia Caregiver. Alzheimer’s Association.
- H. Wang. Lecture: Dementia Care during the COVID-19 Outbreak in China. International Psychogeriatric Association. 2020.



