Introduction
Head and neck cancer is, depending on the study cited, either the 6th or 7th most common malignancy globally, with the majority (~90% of cases) presenting as oral squamous cell carcinoma [1, 2]. Incidence of HNC continues to increase, driven partly by exposure to alcohol, tobacco, and other substances in developing countries and by HPV in developed countries by as much as 30% by 2030, according to one prediction [2]. Men are affected twice as commonly as women, and diagnosis most often occurs after the age of 50 [2]. In the US, the incidence of HNC among males 65+ is estimated at 60:100,000, with a 5-year survival rate of 57% after diagnosis [1]. These patients are in all our practices before, during, and after treatment. Aside from appropriate examination, diagnosis, and referral, dentists are also responsible for understanding the long-term impacts and side effects of both cancer and its treatment. One key finding in many patients that can be disabling and change a patient’s life is pain, particularly chronic neuropathic pain.
What is Neuropathic Pain?
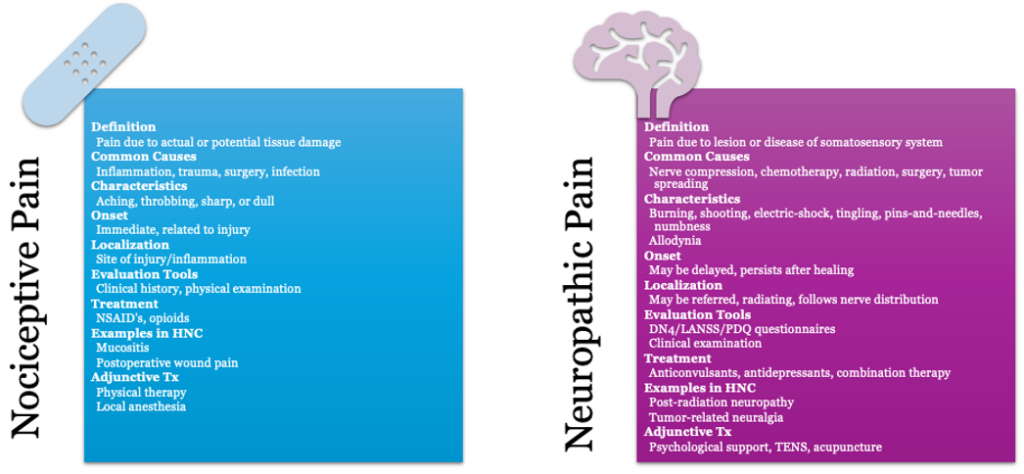
In healthy individuals, pain is experienced as a warning sign in response to actual or potential tissue damage. As the tissue heals, the pain level should improve. Neuropathic pain, however, usually occurs in the absence of tissue damage as a result of a lesion or dysfunction of the somatosensory system – i.e., the part of the central nervous system including bodily senses such as pressure, pain, vibration, temperature, proprioception, and movement [3, 4]. The International Association for the Study of Pain (IASP) defines neuropathic pain as “Neuropathic pain is pain that arises as a direct consequence of a lesion or disease affecting the somatosensory system” [3]. This definition encompasses a wide range of peripheral and central disorders, but it is important to note that not every individual with a lesion will develop a neuropathic pain disorder; the lesion induces changes peripherally and centrally that lead to the pain experienced. The prevalence of neuropathic pain in the general population is estimated at 7-8%, and in individuals with chronic pain, 20-25% [3].
Clinically, neuropathic pain can be distinguished from other types of pain by certain key descriptors. Patients will often complain of electric or shock-like pain, burning, and pain to light touch or movement. They may also experience tingling, pins-and-needles, or numbness in the area. The pain may be continuous, spontaneous, paroxysmal, or evoked. Examination involves testing along the pathway of affected nerves to determine the location and extent of sensory disturbances. There are also screening questionnaires, particularly the LANSS, PDQ, and DN4, that have shown validity in identifying patients with neuropathic pain [1].
How Prevalent is Neuropathic Pain in Head and Neck Cancer?
Neuropathic pain affects 30-40% of all cancer patients, with head and neck cancer (HNC) patients experiencing particularly high rates, up to 80% have pain before treatment, and over 50% report neuropathic-type pain [5, 6]. This pain results from direct tumor invasion of nerves, neurotoxic chemotherapy, or nerve damage from radiation and surgery. Pain often drives patients to seek initial treatment and is frequently the primary presenting symptom [6].
A 2010 systematic review found that 50% of HNC patients experience pain before treatment, 81% during therapy, and 36% at six months post-treatment—with one-third continuing to have pain beyond six months [8]. Patients with neuropathic pain experience more severe symptoms, including breakthrough pain, depression, and insomnia, with pain often lasting longer and being more intense than the original cancer pain [7]. Combination therapies produce the highest pain levels, which can remain elevated for over a year and may never return to baseline [8]. Despite this prevalence, cancer-related pain remains under-reported, under-diagnosed, and under-treated [10].
Recent research by graduate student Sumaia Jaber analyzed data from the NIH All of Us database, studying 39 head and neck cancer patients with neuropathic pain. The findings revealed that combination therapy (surgery, chemotherapy, and radiation together) caused the most nerve-related complications, responsible for 58% of facial neuropathies and over 80% of sensory disturbances. Individual treatments showed lower rates: surgery contributed to 37% of disorders, radiation to 36%, and chemotherapy to 27%. This data confirms that while combination therapy is common in head and neck cancer treatment, it significantly increases the risk of long-term nerve damage and pain compared to single treatments. [11].
Like what you’re learning? Download a brochure for our Orofacial Pain and Oral Medicine certificate or master’s degree program.
What Treatment Options Exist?
The first step in treatment is diagnosis and pain evaluation. Neuropathic and nociceptive pain require different management strategies. There is no “gold-standard” test for diagnosing neuropathic pain, once secondary causes such as tumor or neoplasia have been ruled out; the diagnosis is based on history, clinical examination, and validated questionnaires as mentioned above [12]. Patients can present either positive symptoms, such as tingling, burning, electric shock sensations, or allodynia and hyperpathia in response to stimuli, or negative symptoms like numbness, sensory loss, reduced reflexes, and motor weakness. They may also present hypoesthesia to touch, temperature, paradoxical hypoalgesia to pain, hyperalgesia to pinprick or pressure, and allodynia to cold, heat, or light touch. [7].
A common comorbidity of both pain and cancer that can greatly affect and change outcomes is depression. 20-40% of patients with HNC present with depression, and patients with pre-cancer depression have a reduced survival rate and worse disease progression [13]. HNC patients may also experience other neuropsychological symptoms, including fatigue, sleep disturbance, and cognitive impairment, that can persist beyond 1-year post-treatment and may be associated with other inflammatory markers [14]. These patients may be more somatically focused and require higher levels of analgesics. Effective assessment and treatment of depression, both pharmacologically and non-pharmacologically is crucial, as it can reduce analgesic needs, support cessation of pain-exacerbating habits like tobacco and alcohol use, and ultimately improve overall clinical outcomes [6].
Once a diagnosis is made and comorbidities are identified and treated, there are a number of treatment options that have shown some efficacy for neuropathic pain in the HNC patient. Gabapentin, an anticonvulsant with many years of robust clinical data, reduced neuropathic pain in 5/6 studies in HNC patients [10]. The first-line therapies include pregabalin and gabapentin, particularly in combination with TCA’s or SNRI’s such as amitriptyline or duloxetine [5, 7, 10]. There is some evidence for the use of opioids, but the risk of toxicity is high; possibly a lower dose of opioid could be used in conjunction with an anticonvulsant or antidepressant listed above [5, 7, 10]. TENS and acupuncture have been posited as possible adjunctive therapies, but evidence is not yet robust [5]. There is growing interest in the use of cannabinoids for neuropathic cancer pain, but patients should be cautioned that evidence is lacking, and that there is some evidence that cannabis can stimulate tumor growth, as well as evidence that smoked cannabis can be associated with growth of pulmonary aspergillus in immune-compromised patients [7].
Conclusion
Neuropathic pain affects an important number of head and neck cancer patients yet remains underdiagnosed and under-treated. This chronic pain significantly impacts quality of life and can persist long after treatment ends, particularly following combination therapies. As head and neck cancer rates continue to rise, dentists will increasingly encounter these patients in practice. Early recognition of neuropathic pain symptoms, prompt referral to specialists, and participation in multidisciplinary care teams are essential. By understanding treatment options, from anticonvulsants like gabapentin to addressing comorbid depression, dentists can play a vital role in improving patient outcomes and quality of life.
Earn an Online Postgraduate Degree in Orofacial Pain and Oral Medicine
Are you interested in a variety of issues focused on orofacial pain, medicine and sleep disorders? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Orofacial Pain and Oral Medicine.
References
- Sarode, G., Maniyar, N., Sarode, S. C., Jafer, M., Patil, S., & Awan, K. H. (2020). Epidemiologic aspects of oral cancer. Disease-a-Month, 66(12), 100988. https://doi.org/10.1016/j.disamonth.2020.100988
- Gormley M, Creaney G, Schache A, Ingarfield K, Conway DI. Reviewing the epidemiology of head and neck cancer: definitions, trends and risk factors. Br Dent J. 2022 Nov;233(9):780-786. doi: 10.1038/s41415-022-5166-x. Epub 2022 Nov 11. PMID: 36369568; PMCID: PMC9652141.
- Bouhassira D. (2019). Neuropathic pain: Definition, assessment and epidemiology. Revue neurologique, 175(1-2), 16–25. https://doi.org/10.1016/j.neurol.2018.09.016
- Daly, B. P., Eichen, D. M., Bailer, B., Brown, R. T., & Buchanan, C. L. (2012). Central nervous system. In V. S. Ramachandran (Ed.), Encyclopedia of human behavior (2nd ed., pp. 454–459). Academic Press. https://doi.org/10.1016/B978-0-12-375000-6.00084-7https://www.iasp-pain.org/advocacy/global-year/neuropathic-pain/
- Mulvey, M. R., Paley, C. A., Schuberth, A., King, N., Page, A., & Neoh, K. (2024). Neuropathic Pain in Cancer: What Are the Current Guidelines?. Current treatment options in oncology, 25(9), 1193–1202. https://doi.org/10.1007/s11864-024-01248-7
- Byrd, H. F., & Kohutek, Z. A. (2024). Painful Realities: Navigating the Complexities of Head and Neck Cancer Pain. Oral diseases, 10.1111/odi.15150. Advance online publication. https://doi.org/10.1111/odi.15150
- Davis M. P. (2018). Cancer-Related Neuropathic Pain: Review and Selective Topics. Hematology/oncology clinics of North America, 32(3), 417–431. https://doi.org/10.1016/j.hoc.2018.01.005
- Epstein, J. B., Hong, C., Logan, R. M., Barasch, A., Gordon, S. M., Oberle-Edwards, L., McGuire, D., Napenas, J. J., Elting, L. S., Spijkervet, F. K., & Brennan, M. T. (2010). A systematic review of orofacial pain in patients receiving cancer therapy. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer, 18(8), 1023–1031. https://doi.org/10.1007/s00520-010-0897-7
- Pacheco, R., Cavacas, M. A., Mascarenhas, P., Oliveira, P., & Zagalo, C. (2021). Incidence of Oral Mucositis in Patients Undergoing Head and Neck Cancer Treatment: Systematic Review and Meta-Analysis. Medical Sciences Forum, 5(1), 23. https://doi.org/10.3390/msf2021005023
- Kouri, M., Rekatsina, M., Vadalouca, A., Siafaka, I., Vardas, E., Papadopoulou, E., Paladini, A., & Varrassi, G. (2022). Pharmacological Management of Neuropathic Pain after Radiotherapy in Head and Neck Cancer Patients: A Systematic Review. Journal of clinical medicine, 11(16), 4877. https://doi.org/10.3390/jcm11164877
- Jaber, S. Vistoso A (2025). Cancer-Therapy-Induced Neuropathic & Neurovascular Disorders in the Head & Neck Area. Capstone Form (In process for publication). Orofacial Pain and Oral Medicine, University of Southern California.
- Mulvey, M. R., Boland, E. G., Bouhassira, D., Freynhagen, R., Hardy, J., Hjermstad, M. J., Mercadante, S., Pérez, C., & Bennett, M. I. (2017). Neuropathic pain in cancer: systematic review, performance of screening tools and analysis of symptom profiles. British journal of anaesthesia, 119(4), 765–774. https://doi.org/10.1093/bja/aex175
- Huang, R. W., Chang, K. P., Marchi, F., Loh, C. Y. Y., Lin, Y. J., Chang, C. J., & Kao, H. K. (2022). The impact of depression on survival of head and neck cancer patients: A population-based cohort study. Frontiers in oncology, 12, 871915. https://doi.org/10.3389/fonc.2022.871915
- Amirkhanzadeh Barandouzi, Z., Bruner, D. W., Miller, A. H., Paul, S., Felger, J. C., Wommack, E. C., Higgins, K. A., Shin, D. M., Saba, N. F., & Xiao, C. (2023). Associations of inflammation with neuropsychological symptom cluster in patients with Head and neck cancer: A longitudinal study. Brain, behavior, & immunity – health, 30, 100649. https://doi.org/10.1016/j.bbih.2023.100649



