Temporomandibular disorders (TMDs) are a group of conditions that affect the temporomandibular joint (TMJ), masticatory muscles, and surrounding tissues, resulting in pain, limited jaw movement, and joint noises such as clicking or popping. TMDs represent one of the most common causes of orofacial pain and significantly impact the quality of life for affected individuals. Despite the prevalence of these conditions, their diagnosis and management have traditionally been underemphasized in dental education.
Recognizing this gap, the Commission on Dental Accreditation (CODA) revised its standards in 2020 by mandating the inclusion of TMD education in the predoctoral curriculum of all U.S. dental schools by 2022 (Commission on Dental Accreditation, 2020). In 2021 the American Academy of Orofacial Pain (AAOP) responded by developing a comprehensive framework to integrate TMD education into dental programs, offering a structured and evidence-based approach for teaching students about the diagnosis, evaluation, and management of TMDs.
Like what you’re learning? Download a brochure for our Orofacial Pain and Oral Medicine certificate or master’s degree program.
The Importance of TMD Education
TMDs are a widespread public health concern, affecting approximately 5-12% of the population at any given time, with women being disproportionately affected. Symptoms can range from mild discomfort to debilitating pain, significantly interfering with daily activities such as chewing, speaking, and sleeping. As general dentists are often the first healthcare providers consulted by patients with TMD, it is essential that dental professionals have the necessary knowledge and skills to address these conditions effectively (Figure 1).
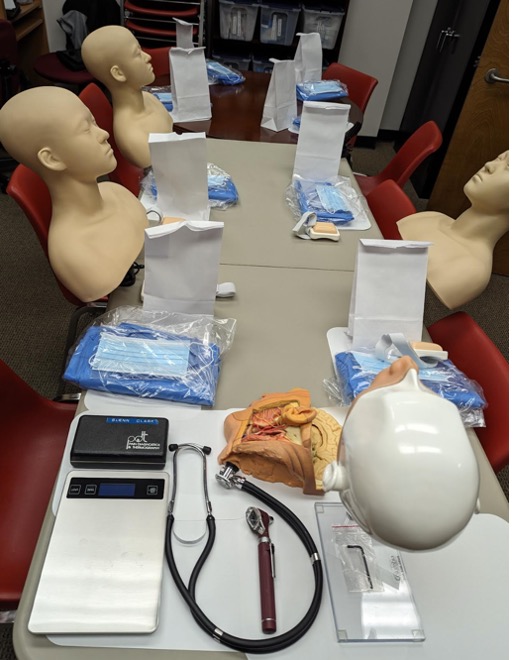
Figure 1. Shows the preparation and resources for pre-clinical session on TMD for dental students.
Historically, TMD education has been fragmented, often relegated to elective courses or postdoctoral programs. This lack of structured training has left many dental graduates underprepared to diagnose and manage TMDs, leading to underdiagnosis, mismanagement, and patient frustration. Integrating TMD education into the predoctoral curriculum ensures that future dentists are equipped to provide comprehensive care and prevent chronic orofacial pain.
The AAOP’s recommended framework is aligned with CODA’s classification of biomedical, behavioral, and clinical science knowledge, as well as the American Dental Education Association’s (ADEA) domains for dental competencies:
- Critical Thinking
- Professionalism
- Communication and Interpersonal Skills
- Health Promotion
- Practice Management and Informatics
- Patient Care, including assessment, diagnosis, treatment planning, and maintenance of oral health.
The AAOP framework divides TMD education into five key domains:
1. Knowledge Base of TMDs and Orofacial Pain
The first domain focuses on building a strong foundation of knowledge regarding the basic science, mechanisms, and etiologies of TMDs. Students must understand the anatomical, physiological, and neurological aspects of the TMJ and surrounding structures, as well as the pathophysiology of TMDs. This knowledge allows dental professionals to identify preventive strategies based on current evidence and integrate them into routine dental care.
2. Screening, Evaluation, Diagnosis, and Risk Assessment
Early and accurate diagnosis is critical for preventing the progression of TMDs. The AAOP recommends that dental students be trained to conduct systematic screening and risk assessments for TMDs as part of routine dental examinations.
Training includes:
- Identifying TMD symptoms like pain, joint noises, and limited jaw function
- Assessing risk factors, including stress, parafunctional habits, trauma, and systemic diseases
- Understanding when to refer patients to specialists for further evaluation
3. Health Promotion and Prevention of TMDs
Prevention is a cornerstone of modern dentistry, and TMD education should emphasize strategies for reducing the risk of developing TMDs (AAOP, 2021). Students must learn to educate patients about lifestyle modifications and behavioral interventions that can mitigate TMD symptoms, such as:
- Avoiding parafunctional habits (e.g., teeth grinding or nail-biting)
- Managing stress through relaxation techniques
- Practicing proper jaw posture and ergonomics
4. Clinical Decision-Making, Treatment Planning, and Evidence-Based Management
This domain focuses on equipping students with the clinical reasoning skills necessary to develop and implement effective treatment plans for TMD patients. The AAOP emphasizes the importance of evidence-based practice, where clinical decisions are guided by the latest research and best practices.
Key components include:
- Non-invasive treatments such as self-management strategies, physical therapy, and oral appliances
- Pharmacological interventions for pain management
- Recognizing the role of interdisciplinary collaboration with specialists such as oral surgeons, physical therapists, and pain management experts
5. Practice Management and Informatics
Integrating TMD management into general practice requires efficient practice management and the use of informatics. Dental students must learn to:
- Document TMD assessments and treatments accurately.
- Utilize digital tools for diagnosis and patient education
- Manage TMD cases within the broader context of dental practice
Implications for the Future of Dental Practice
The integration of TMD education into predoctoral curricula represents a significant advancement for dental education and clinical practice. Equipping dental students with the knowledge and skills to diagnose and manage TMDs not only enhances clinical competency, but also strengthens the role of general dentists in addressing orofacial pain, ultimately improving patient outcomes and advancing the standard of care.
Earn an Online Postgraduate Degree in Orofacial Pain and Oral Medicine
Are you interested in a variety of issues focused on orofacial pain, medicine and sleep disorders? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Orofacial Pain and Oral Medicine.
References
- https://www.nidcr.nih.gov/health-info/tmd).
- De Leeuw, R. and Klasser, G.D. (2018) Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management. 6th Edition, Quintessence, Chicago
- Okeson, J. P. (2020). Management of temporomandibular disorders and occlusion (8th ed.). Elsevier.
- Wright, E. F., & Klasser, G. D. (2020). Manual of temporomandibular disorders (4th ed.). Wiley-Blackwell.
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Board on Health Sciences Policy; Committee on Temporomandibular Disorders (TMDs): From Research Discoveries to Clinical Treatment; Yost O, Liverman CT, English R, et al., editors. Temporomandibular Disorders: Priorities for Research and Care. Washington (DC): National Academies Press (US); 2020 Mar 12. 6, Improving TMD Health Care: Practice, Education, Access, and Coverage. https://www.ncbi.nlm.nih.gov/books/NBK557987/


