Painful temporomandibular disorder (TMD) stands as a prevalent source of orofacial pain, affecting 5-12% of US adults. As dentists, our encounters with TMD cases are frequent, with patients presenting discomfort, audible sounds, or limitations in jaw movement. Despite its subtle nature, TMD significantly impacts daily life, urging us to delve into a comprehensive understanding [1].
Root Causes and Complexity
The elusive nature of TMD’s root causes often leaves us grappling for explanations. Factors such as excessive strain on the jaw joints (commonly associated with bruxism), arthritis, displaced jaw joint articular disc, or concurrent systemic medical conditions such as fibromyalgia, rheumatoid arthritis, systemic lupus erythematosus, among others, can contribute to the complexity of TMD pain [2].
Beyond Physical Discomfort
TMD pain extends beyond physical discomfort, permeating daily life and giving rise to secondary symptoms like cephalalgias, cervicodynia, and sleep disturbances. Our focus transcends mere symptom relief and restoring control over daily functions [3].
Like what you’re learning? Download a brochure for our Orofacial Pain and Oral Medicine certificate or master’s degree program.
Connecting Rheumatoid Conditions and TMJ Manifestations
Recognizing the potential link between rheumatoid conditions and TMJ manifestations becomes imperative, as well as the elucidation of the signs and symptoms acting as red flags, reflecting the need to suspect rheumatologic conditions. It underscores the pivotal role of rheumatologists in managing TMJ pain, providing valuable insights for our dental practice [4].
The Temporomandibular joint sits just in front of the ear. The mandibular condylar head articulates against the glenoid fossa with an interposed fibro-cartilaginous articular disc (Figure 1), allowing smooth, pain-free joint function.
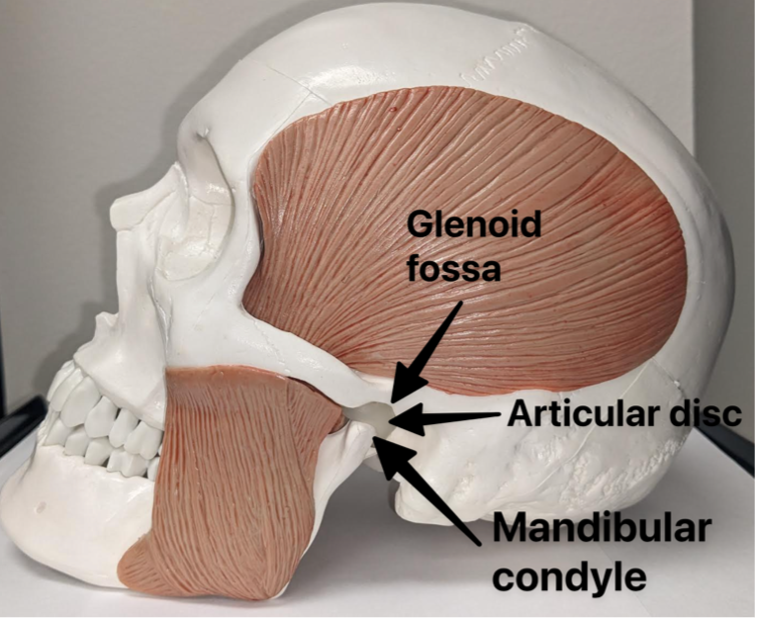
Figure 1. Anatomy model showing the temporal and masseter muscle with black arrows pointing to the mandibular condyle, articular disc, and glenoid fossa.
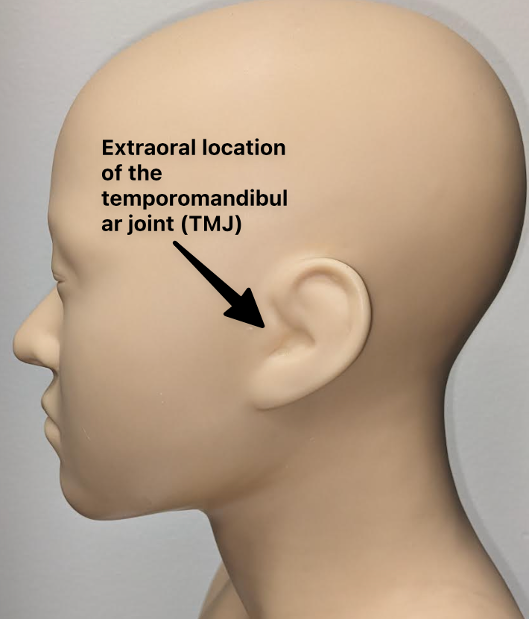
Figure 2. Mannequin with a black arrow showing the extraoral location of the TMJ (temporomandibular joint) in front of the ear.
Signs and Symptoms of TMD
Patients commonly present with temporomandibular disorder (TMD), manifesting as orofacial discomfort during mastication, phonation, or rest. Audible temporomandibular joint (TMJ) sounds (Figure 2), such as clicking or popping, may also be reported. Restriction of jaw movement, indicative of limitations in range of motion, is frequently observed. However, some cases need a multidisciplinary approach, and thorough evaluation by a rheumatologist is indicated.
Multidisciplinary Approach
A multidisciplinary approach is crucial in diagnosing and treating temporomandibular disorders (TMD), emphasizing the need for collaboration between dental practitioners and rheumatologists. Dental professionals should prompt patients with persistent TMJ symptoms to seek timely medical consultation, guiding them toward appropriate channels for comprehensive evaluation. Diagnosis entails thoroughly reviewing the patient’s medical and dental history, including exploring psychosocial stressors and pre-existing conditions.
Rheumatologist Evaluation should be considered, but not limited to the following cases:
Patients with systemic manifestations, including widespread arthralgia, fatigue, or joint swelling, may consider consulting a rheumatologist. Rheumatological expertise is indispensable for thoroughly evaluating potential systemic implications in TMD cases[5].
- Patients with possible autoimmune-mediated TMJ involvement, as seen in conditions like rheumatoid arthritis or lupus, underscores the significance of rheumatological consultation. Rheumatologists specialize in managing autoimmune disorders, ensuring precise diagnosis and tailored therapeutic interventions [6].
- Patient with connective tissue disorders, exemplified by Ehlers-Danlos syndrome or scleroderma, exerting effects on TMJ structures, mandate rheumatological assessment. Rheumatologists are adept at addressing complex connective tissue pathologies, contributing nuanced perspectives to the overall management strategy [6].
- Failed Conservative Management: In instances where conventional therapeutic modalities, such as lifestyle modifications and standard pharmacotherapy, prove ineffective, a rheumatological consult is prudent. Rheumatologists bring alternative approaches and pharmacological interventions tailored to the specific etiology of TMJ pathology [7].
- When diagnostic ambiguity persists or when there is suspicion of an underlying rheumatologic etiology, collaborative evaluation with a rheumatologist is judicious. This combined effort ensures a precise diagnosis and targeted therapeutic interventions [8].
- Young Patients with Early Onset of TMJ Pain and/or Asymmetry: Early onset of TMJ symptoms in the young demographic, particularly when accompanied by asymmetry, merits rheumatological scrutiny. Rheumatologists proficiently assess and manage systemic conditions that may present with orofacial manifestations in younger populations [8,9].
Lab Tests and Exam Considerations
Clinical examination, encompassing assessment of TMJ range of motion, palpation of TMJ structures, and evaluation of dental occlusion, aids in identifying specific pathologies contributing to TMJ symptoms (10). Integration of advanced diagnostic modalities, such as panoramic radiographs, cone-beam computed tomography (CBCT), magnetic resonance imaging (MRI), autoimmunity serologic tests ( for instance, but not limited to antinuclear antibody [ANA], rheumatoid factor [RF], Anti-cyclic citrullinated peptide [anti-CCP], C-reactive protein, erythrocyte sedimentation rate [ESR], Anti–Sjögren syndrome antigen A and B [anti-SSA, anti-SSB]), bone scintigraphy are part of the available and possibly diagnostic tools for interpreting the multifactorial nature of TMD and formulating tailored treatment regimens. Rheumatologist consultation and evaluation should be considered in cases involving systemic manifestations, autoimmune-mediated TMJ involvement, connective tissue disorders, failed conservative management, diagnostic ambiguity, or early onset of symptoms in young patients, ensuring a comprehensive and targeted approach to care [7,8 10].
Conclusion
Recognizing TMD as more than local discomfort is crucial. Cooperative efforts with rheumatologists become preeminent when faced with complex TMD cases, ensuring a holistic approach to understanding underlying causes and implementing targeted interventions. Their expertise in musculoskeletal intricacies aids in understanding underlying causes and managing interventions for those facing systemic complexities, marking an influence in collaborative healthcare opportunities.
Earn an Online Postgraduate Degree in Orofacial Pain and Oral Medicine
Are you interested in a variety of issues focused on orofacial pain, medicine and sleep disorders? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Orofacial Pain and Oral Medicine.
References
- Management of temporomandibular joint disorders: A surgeon’s perspective. Dimitroulis 1 PMID: 29574810 DOI: 10.1111/adj.12593
- Temporomandibular Syndrome. Kushagra Maini; Anterpreet Dua.Last Update: January 30, 2023.
- Temporomandibular Joint Disorders: A Review of Etiology, Clinical Management, and Tissue Engineering Strategies Meghan K. Murphy, BE,a Regina F. MacBarb, BS,a Mark E. Wong, DDS,b and Kyriacos A. Athanasiou, PhD, PEa,* Int J Oral Maxillofac Implants. 2013 Nov-Dec; 28(6): e393–e414. doi: 10.11607/jomi.te20 PMCID: PMC4349514 NIHMSID: NIHMS661047PMID: 24278954
Temporomandibular joint involvement in rheumatoid arthritis patients: association between clinical and tomographic data Patrícia Cf Cordeiro 1 , Josemar P Guimaraes 2 , Viviane A de Souza 3 , Isabela M Dias 2 , Jesca Nn Silva 2 , Karina L Devito 2 , Leticia L Bonato 4 PMID: 28383601 - Temporomandibular joint involvement in rheumatoid arthritis patients: association between clinical and tomographic data Patrícia Cf Cordeiro 1 , Josemar P Guimaraes 2 , Viviane A de Souza 3 , Isabela M Dias 2 , Jesca Nn Silva 2 , Karina L Devito 2 , Leticia L Bonato 4 PMID: 28383601
- Main Oral Manifestations in Immune-Mediated and Inflammatory Rheumatic DiseasesJ. Clin. Med. 2019, 8(1), 21; https://doi.org/10.3390/jcm8010021
- Nonsurgical management of temporomandibular joint autoimmune disorders Ehsan Shoohanizad,1 Ata Garajei,2 Aida Enamzadeh,3 and Amir Yari2,* doi:10.3934/publichealth.2019.4.554 PMCID: PMC6940567 PMID: 3190907
- Covert L, Mater HV, Hechler BL. Comprehensive Management of Rheumatic Diseases Affecting the Temporomandibular Joint. Diagnostics. 2021; 11(3):409. https://doi.org/10.3390/diagnostics11030409
- Shim, J.S., Kim, C., Ryu, J.J. et al. Correlation between TM joint disease and rheumatic diseases detected on bone scintigraphy and clinical factors. Sci Rep 10, 4547 (2020). https://doi.org/10.1038/s41598-020-60804-x
- González-Chávez SA, Pacheco-Tena C, de Jesús Caraveo-Frescas T, Quiñonez-Flores CM, Reyes-Cordero G, Campos-Torres RM. Oral health and orofacial function in patients with rheumatoid arthritis. Rheumatol Int. 2020 Mar;40(3):445-453. doi: 10.1007/s00296-019-04440-3. Epub 2019 Sep 17. PMID: 31531708.
- Hysa E, Lercara A, Cere A, Gotelli E, Gerli V, Paolino S, Pizzorni C, Sulli A, Smith V, Cutolo M. Temporomandibular disorders in immune-mediated rheumatic diseases of the adult: A systematic review. Semin Arthritis Rheum. 2023 Aug;61:152215. doi: 10.1016/j.semarthrit.2023.152215. Epub 2023 May 5. PMID: 37167773.

